Colorectal Cancer Awareness Month:The Importance of Routine Screening
Colorectal Cancer Awareness Month, observed every March, serves as a crucial reminder of the importance of early detection and prevention.
Colorectal cancer (CRC) is one of the leading causes of cancer-related deaths worldwide, but it is also one of the most preventable and treatable when caught early.
Routine screening plays a vital role in detecting precancerous polyps and diagnosing CRC in its early stages, significantly improving survival rates.
In this article, we will explore the significance of Colorectal Cancer Awareness Month, the risk factors for CRC, different screening methods, and why routine screenings can save lives.
Understanding Colorectal Cancer
Colorectal cancer affects the colon (large intestine) and rectum, developing from abnormal growths called polyps.
While some polyps remain benign, others can become cancerous over time. Early detection of these polyps through screening allows for their removal before they progress into cancer.
Global Impact of Colorectal Cancer
- CRC is the third most common cancer
- It is the second leading cause of cancer-related deaths in both men and women in many countries.
- The survival rate is over 90% when detected early, but it drops significantly if diagnosed at a later stage.
Despite these statistics, many people still do not undergo regular screenings, often due to a lack of awareness, fear, or misinformation. This is why Colorectal Cancer Awareness Month is crucial—it educates the public on the importance of early detection and prevention.

Risk Factors for Colorectal Cancer
1. Age
The risk of CRC increases with age, with most cases occurring in individuals over 50. However, recent studies show a concerning rise in young-onset colorectal cancer, emphasizing the need for awareness among younger populations.
2. Family History and Genetics
A family history of colorectal cancer or polyps increases the risk. Individuals with inherited syndromes like Lynch syndrome or familial adenomatous polyposis (FAP) have a much higher chance of developing CRC.
3. Lifestyle Factors
- Diet: A high intake of processed and red meats, combined with low fiber consumption, has been linked to an increased risk.
- Lack of Physical Activity: A sedentary lifestyle contributes to obesity, which is a known risk factor.
- Smoking and Alcohol Consumption: Long-term tobacco use and excessive alcohol intake elevate the risk of CRC.
4. Medical Conditions
- Inflammatory Bowel Disease (IBD): Conditions like Crohn’s disease and ulcerative colitis increase CRC risk due to chronic inflammation.
- Diabetes: Individuals with type 2 diabetes have a higher risk of developing colorectal cancer.
By understanding these risk factors, individuals can make informed choices to lower their chances of developing CRC through lifestyle changes and regular screenings.

Why Routine Screening Matters
Screening is essential because colorectal cancer can develop silently without noticeable symptoms in its early stages.
By the time symptoms appear, the disease may have already advanced, making treatment more challenging.
Benefits of Routine Screening
- Early Detection: Finds cancer before symptoms develop, when it is easier to treat.
- Prevention: Identifies and removes precancerous polyps before they turn cancerous.
- Increased Survival Rates: Early-stage CRC has a 90% five-year survival rate, whereas late-stage CRC survival drops to 14%.
- Less Invasive Treatments: Early detection may allow for minimally invasive treatments instead of major surgery.
Colorectal Cancer Screening Methods
Several screening tests can help detect colorectal cancer and polyps. The most suitable test depends on individual risk factors and medical history.
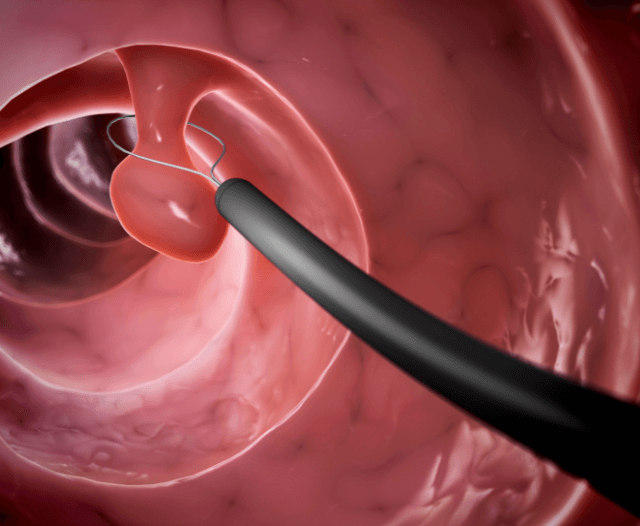
1. Colonoscopy (Gold Standard)
What It Is: A procedure in which a long, flexible tube with a camera is inserted into the colon to examine for polyps or cancer.
Why It’s Important: It is the most comprehensive screening tool, allowing doctors to detect and remove polyps during the same procedure.
How Often: Every 10 years for individuals at average risk, or more frequently for high-risk individuals.
These tests detect hidden blood or DNA changes in the stool that may indicate cancer.
Fecal Immunochemical Test (FIT)
What It Is: A simple, non-invasive test that detects blood in the stool.
How Often: Annually.
Guaiac-Based Fecal Occult Blood Test (gFOBT)
What It Is: Another stool test that detects blood, but requires dietary restrictions before testing.How Often: Annually.
Cologuard (Multitarget Stool DNA Test)
What It Is: Detects DNA changes associated with cancer in stool samples.
How Often: Every 3 years.
What It Is: Similar to a colonoscopy but only examines the lower part of the colon.
How Often: Every 5 years, or every 10 years if combined with FIT.
4. CT Colonography (Virtual Colonoscopy)
What It Is: A specialized CT scan that creates detailed images of the colon.
How Often: Every 5 years.
While less invasive, stool-based tests and CT colonography do not allow for immediate polyp removal, meaning a follow-up colonoscopy may be necessary.

Overcoming Barriers to Screening
Despite the benefits, many people delay or avoid CRC screening. Common reasons include:
- Fear of Discomfort: Colonoscopy prep may be unpleasant, but it is a small price to pay for potentially life-saving early detection.
- Lack of Awareness: Many people underestimate their risk or do not realize the importance of screening.
- Access and Cost: Screening may not always be readily available. However, many health programs offer free or low-cost options.
To increase participation, healthcare providers and advocacy groups must continue educating the public and making screening accessible to all.
The Role of Colorectal Cancer Awareness Month
This annual campaign focuses on:
Raising Awareness: Educating the public about risk factors and symptoms.
Encouraging Screenings: Reminding people to schedule their routine colonoscopies or stool tests.
Supporting Research: Funding initiatives to improve early detection and treatment options.
Honoring Survivors: Celebrating those who have overcome colorectal cancer and advocating for continued research.
Events such as awareness walks, free screening programs, and social media campaigns play a crucial role in spreading the message.
What You Can Do to Protect Yourself
Know Your Risk: Discuss your family history and risk factors with your doctor.
Get Screened: Follow recommended screening guidelines for your age and risk level.
Adopt a Healthy Lifestyle: Eat a balanced diet, exercise regularly, and avoid smoking and excessive alcohol consumption.
Spread Awareness: Encourage friends and family to prioritize screening.

Conclusion
Colorectal Cancer Awareness Month is more than just a campaign—it is a life-saving movement. Routine screenings are the most effective way to detect colorectal cancer early and even prevent it altogether.
By prioritizing your health and encouraging others to do the same, you can help reduce the burden of this disease.
Don’t wait—schedule your screening today. Early detection saves lives!
By promoting awareness, education, and proactive screening, we can work together to combat colorectal cancer and improve survival rates worldwide.
Get in Contact with Dr. Deetlefs
Gi Doc Capetown is a practice founded to provide medical solutions in the area of gastroenterology.
Over the years, Dr Eduan Deetlefs has earned the reputation of a trusted health expert providing consultative, diagnostic, and therapeutic endoscopic and related services to patients in
Cape Town and beyond.
If you would like to book an appointment with a gastrointestinal (GI) specialist or would simply like more information on a particular GI topic, don’t hesitate to use our online booking form or call Dr. Deetlefs at 021 551 867.
DISCLAIMER: PLEASE READ CAREFULLY
The information on this website is to provide general guidance. In no way does any of the information provided reflect definitive medical advice and self-diagnoses should not be made based on information obtained online. It is important to consult a Gastroenterologist or medical doctor regarding ANY and ALL symptoms or signs including, but not limited to: abdominal pain, haemorrhoids or anal / rectal bleeding as it may a sign of a serious illness or condition. A thorough consultation and examination should ALWAYS be performed for an accurate diagnosis and treatment plan. Be sure to call a physician or call our office today and schedule a consultation.
© Dr. Eduan Deetlefs, Registered Gastroenterologist, GI Doc Cape Town
Our website information is not intended or implied to be a substitute for professional medical advice, diagnosis or treatment. Please consult a doctor about your specific condition. Only a trained physician can determine an accurate diagnosis and proper treatment.