Gastrointestinal (GI) obstruction is a serious condition that can significantly impact digestion and overall health. Whether caused by tumors, strictures, inflammation, or other factors, GI obstructions can block the passage of food, fluids, and waste through the digestive tract. In such cases, restoring the flow through the gastrointestinal system becomes an urgent medical necessity. One of the most effective, minimally invasive solutions is endoscopic stent placement.
This article explores what endoscopic stent placement is, why it’s used, how the procedure is performed, and what patients can expect before, during, and after treatment. Understanding this procedure can empower patients and caregivers to make informed decisions about their GI care.
What Is GI Obstruction?
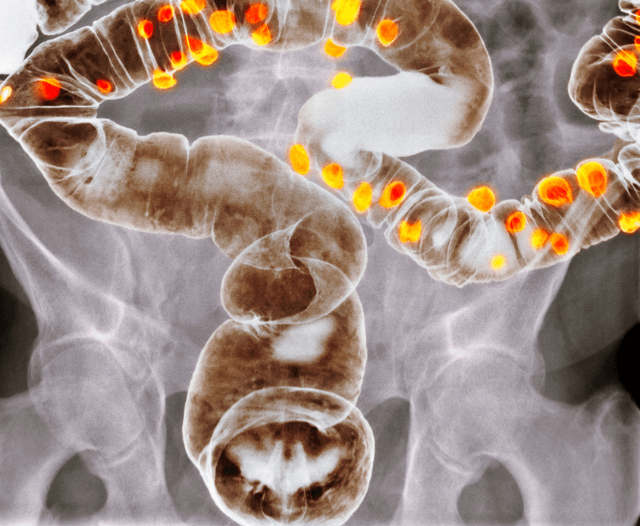
GI obstruction occurs when the normal movement of contents through the digestive tract is blocked. This can happen in the esophagus, stomach, small intestine, colon, or rectum. Obstructions can be either partial or complete, and causes may include:
- Malignant tumors (such as colorectal, gastric, or pancreatic cancer)
- Benign strictures due to inflammation, ulcers, or surgery
- Diverticulitis
- Crohn’s disease
- Radiation-induced narrowing
- Foreign objects
Symptoms may include nausea, vomiting, abdominal pain, constipation, bloating, and inability to pass gas or stool.
What Is Endoscopic Stent Placement?
Endoscopic stent placement is a minimally invasive procedure used to treat obstructions in the gastrointestinal tract. A stent is a tube-like device, usually made of metal or plastic, that is inserted into the GI tract to keep a narrowed or blocked area open, allowing for the normal passage of food, fluids, or waste.
Stents can be placed in several areas of the GI tract, including:
- Esophagus – for esophageal cancer or strictures
- Duodenum or small intestine – for gastric outlet obstruction
- Colon – for obstructive colorectal cancer
- Bile ducts – though technically not part of the GI tract, endoscopic stenting is common here too
This procedure is commonly performed using endoscopy, which involves a thin, flexible tube with a camera (endoscope) that allows the doctor to see the inside of the GI tract in real time.
When Is Endoscopic Stent Placement Recommended?
Endoscopic stent placement is typically recommended in the following scenarios:
1. Malignant Obstruction (Cancer)
Many patients with advanced cancers in the GI tract experience obstruction as a complication. A stent can relieve symptoms and improve quality of life. In such cases, it is often used as a palliative measure for patients who are not candidates for surgery.
2. Benign Strictures
In cases of non-cancerous narrowing caused by chronic inflammation (e.g., Crohn’s disease, radiation enteritis), stenting may be used when other treatments such as dilation have failed or if the narrowing is recurrent.
3. Preoperative Bridge to Surgery
In patients with obstructing colon cancer, a stent may be used to decompress the bowel before elective surgery, allowing time for better surgical planning and avoiding emergency surgery.
Types of GI Stents
There are several types of stents used in the gastrointestinal tract:
- Self-expanding metal stents (SEMS): Most commonly used, especially in malignancies.
- Plastic stents: Usually used in benign conditions or temporary placements.
- Covered vs. Uncovered stents:
- Covered stents prevent tumor ingrowth but are more prone to migration.
- Uncovered stents stay in place better but can become obstructed over time by tissue growth.
Your doctor will select the appropriate type based on the location and cause of the obstruction.

The Procedure: What to Expect
1. Preparation
Patients are typically advised not to eat or drink anything for several hours before the procedure. Your doctor may recommend stopping certain medications like blood thinners. You may also receive instructions for bowel preparation if the stent is being placed in the colon.
2. During the Procedure
- You will be given a sedative or anesthesia for comfort.
- An endoscope is inserted through the mouth or rectum, depending on the location of the obstruction.
- Once the narrowed area is visualized, a guidewire is passed through it.
- The stent is then advanced over the guidewire and deployed in the affected area.
- The stent expands on its own (self-expanding) or is manually expanded to keep the passage open.
The procedure usually takes 30 to 60 minutes.
3. After the Procedure
- Patients are monitored for a few hours and can often return home the same day.
- Some may experience mild abdominal discomfort, gas, or bloating.
- Eating and drinking are usually resumed within 24 hours, starting with liquids and advancing to soft foods.
- Follow-up visits are scheduled to monitor the stent’s function and address any complications.
Benefits of Endoscopic Stent Placement
- Minimally invasive
- Quick symptom relief
- Shorter recovery time compared to surgery
- Improves quality of life in palliative care
- Can avoid emergency surgery

Potential Risks and Complications
Although generally safe, endoscopic stent placement does carry some risks, including:
- Stent migration – more common with covered stents
- Perforation – a tear in the wall of the GI tract
- Bleeding
- Stent occlusion – due to tumor ingrowth, food blockage, or tissue overgrowth
- Infection
Complications are usually manageable, and your gastroenterologist will discuss the risks with you before the procedure.
Follow-Up Care and Lifestyle Tips
After a stent is placed, it’s important to:
- Follow dietary recommendations – chew food thoroughly, avoid sticky or fibrous foods, and drink plenty of water
- Attend follow-up appointments – to ensure the stent is functioning well
- Watch for warning signs – such as increasing abdominal pain, vomiting, fever, or difficulty swallowing (depending on location)
If symptoms return, your doctor may perform additional imaging or endoscopy to assess the stent.
Alternatives to Stenting
Depending on your condition, other treatments may be considered:
- Endoscopic balloon dilation – especially for short benign strictures
- Surgical resection – for suitable candidates, especially in cancer cases
- Bypass surgery – for advanced tumors where resection isn’t possible
The best approach depends on the underlying cause, your overall health, and treatment goals.

Conclusion
Endoscopic stent placement is a highly effective, minimally invasive procedure used to relieve GI obstruction caused by tumors, strictures, or other blockages. Whether as a palliative measure in advanced cancer or a temporary solution before surgery, stents can significantly improve comfort and quality of life.
If you or a loved one is experiencing symptoms of GI obstruction, consult a gastroenterologist or GI specialist. Early diagnosis and prompt intervention can lead to better outcomes and a faster return to normal life.
For personalized consultation and expert care, don’t hesitate to reach out to a specialist with experience in advanced endoscopic procedures.
Get in Touch
Dr. Deetlefs has earned the reputation of a trusted health expert providing consultative, diagnostic, and therapeutic endoscopic and related services to patients in Cape Town and beyond.
Dr. Deetlefs can be contacted to confirm the estimated breakdown should you be interested in having the procedure done.
DISCLAIMER: PLEASE READ CAREFULLY
The information on this website is to provide general guidance. In no way does any of the information provided reflect definitive medical advice and self-diagnoses should not be made based on information obtained online. It is important to consult a Gastroenterologist or medical doctor regarding ANY and ALL symptoms or signs including, but not limited to: abdominal pain, haemorrhoids or anal / rectal bleeding as it may a sign of a serious illness or condition. A thorough consultation and examination should ALWAYS be performed for an accurate diagnosis and treatment plan. Be sure to call a physician or call our office today and schedule a consultation.
© Dr. Eduan Deetlefs, Registered Gastroenterologist, GI Doc Cape Town
Our website information is not intended or implied to be a substitute for professional medical advice, diagnosis or treatment. Please consult a doctor about your specific condition. Only a trained physician can determine an accurate diagnosis and proper treatment.