Introduction
Navigating the world of gastrointestinal disorders can be challenging, especially when faced with conditions like Irritable Bowel Syndrome (IBS) and Inflammatory Bowel Disease (IBD).
While both can cause discomfort and disrupt daily life, they are distinct conditions with unique characteristics and treatment approaches.
Understanding the differences between IBS and IBD is crucial for accurate diagnosis and effective management.
In this article, we’ll explore the key distinctions between these two gastrointestinal disorders, including their symptoms, underlying causes, diagnostic methods, and treatment strategies.
By gaining a deeper understanding of IBS and IBD, individuals can better advocate for their health and work with healthcare providers to develop personalized management plans.
Understanding Irritable Bowel Syndrome (IBS)
Irritable Bowel Syndrome is a functional gastrointestinal disorder characterized by a collection of symptoms that can include abdominal pain, bloating, gas, diarrhea, and constipation.
Unlike IBD, IBS does not involve inflammation or structural damage to the intestines. Instead, it is believed to arise from dysregulation of the gut-brain axis, which affects gut motility, sensitivity, and function.
Key Features of IBS
- Symptoms: The hallmark symptoms of IBS include abdominal discomfort or pain that is often relieved by bowel movements, as well as changes in bowel habits such as diarrhea, constipation, or a combination of both.
- Absence of Inflammation: IBS does not cause inflammation or structural damage to the intestines, as seen in IBD.
- Triggers: Certain factors such as stress, dietary choices, hormonal fluctuations, and medications can trigger or exacerbate symptoms of IBS.
- Diagnosis: Diagnosis of IBS is based on the presence of characteristic symptoms and the exclusion of other gastrointestinal conditions. There are no specific diagnostic tests for IBS, but healthcare providers may perform tests to rule out other disorders ie. Colonoscopy or upper endoscopy.
- Treatment: Treatment for IBS focuses on managing symptoms and improving quality of life. This may involve dietary modifications, stress management techniques, medications to relieve symptoms, and lifestyle changes.

Causes of Irritable Bowel Syndrome
The exact cause of Irritable Bowel Syndrome (IBS) remains unknown, and it is likely influenced by a combination of factors. While the precise underlying mechanisms are not fully understood, several potential contributors to IBS have been identified.
These include:
- Altered Gut Motility: Abnormal contractions of the intestinal muscles may lead to changes in bowel habits such as diarrhea, constipation, or alternating between the two.
- Visceral Hypersensitivity: Individuals with IBS may experience heightened sensitivity to stimuli within the gastrointestinal tract, leading to increased perception of pain or discomfort.
- Abnormal Brain-Gut Communication: Dysfunction in the communication between the brain and the gut, known as the gut-brain axis, may play a role in the development of IBS.
- Changes in Gut Microbiota: Alterations in the composition and diversity of the gut microbiota, the community of microorganisms that inhabit the digestive tract, have been observed in individuals with IBS.
- Psychological Factors: Stress, anxiety, depression, and other psychological factors are known to influence gut function and may exacerbate symptoms in individuals with IBS.
- Dietary Factors: Certain foods and dietary components have been implicated as triggers for IBS symptoms in some individuals. Common dietary triggers include high-fat foods, spicy foods, caffeine, alcohol, artificial sweeteners, and foods high in FODMAPs.
- Genetic Predisposition: Family history of IBS or other functional gastrointestinal disorders may predispose individuals to the condition.

Understanding Inflammatory Bowel Disease (IBD)
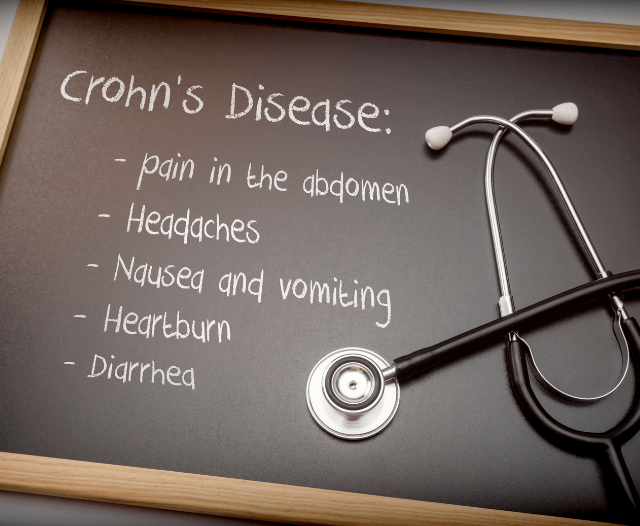
Inflammatory Bowel Disease encompasses two chronic inflammatory conditions of the digestive tract:
Crohn’s disease and Ulcerative Colitis.
Unlike IBS, which is a functional disorder, IBD involves inflammation and damage to the intestinal tissue, leading to complications such as strictures, fistulas, and nutritional deficiencies.
Key Features of IBD
- Symptoms: Symptoms of IBD can vary depending on the type and location of the condition but may include abdominal pain, diarrhea, rectal bleeding, weight loss, fatigue, and fever.
- Inflammation: IBD is characterized by chronic inflammation of the gastrointestinal tract, which can occur anywhere from the mouth to the anus in Crohn’s disease and is typically limited to the colon and rectum in Ulcerative Colitis.
- Chronic Nature: IBD is a chronic condition with periods of active disease (flare-ups) and periods of remission, during which symptoms may improve or disappear.
- Diagnosis: Diagnosis of IBD typically involves a combination of medical history, physical examination, blood tests, imaging studies, and tissue biopsy to assess inflammation and rule out other conditions.
- Treatment: Treatment for IBD aims to reduce inflammation, alleviate symptoms, and prevent complications.
Causes of Irritable Bowel Disease
Irritable Bowel Disease (IBD) is a term that is not typically used in medical literature.
The correct term for chronic inflammatory conditions of the digestive tract is Inflammatory Bowel Disease (IBD). Inflammatory Bowel Disease primarily includes Crohn’s disease and Ulcerative Colitis.
The causes of Inflammatory Bowel Disease (IBD) are complex and not fully understood. However, research suggests that a combination of genetic, environmental, immune, and microbial factors contribute to the development of IBD. Here are some key factors that may play a role:
- Genetic Predisposition: Family history is a significant risk factor for IBD, suggesting a genetic component to the disease.
- Dysregulated Immune Response: In individuals with IBD, the immune system mistakenly attacks the gastrointestinal tract, leading to chronic inflammation. It is thought that a dysregulated immune response, possibly triggered by environmental factors, contributes to the development of IBD.
- Environmental Factors: Various environmental factors have been implicated in the development of IBD, including diet, smoking, antibiotic use, stress, and exposure to certain infections or pollutants.
- Alterations in Gut Microbiota: The gut microbiota, the diverse community of microorganisms that inhabit the digestive tract, plays a crucial role in maintaining intestinal health and immune function.
- Intestinal Barrier Dysfunction: Dysfunction of the intestinal epithelial barrier, which normally acts as a protective barrier against harmful substances and pathogens, has been implicated in the development of IBD. Increased intestinal permeability, or “leaky gut,” may allow harmful substances to penetrate the intestinal lining and trigger an immune response.
- Immunological Triggers: Infections and other immunological triggers may initiate or exacerbate inflammation in the gastrointestinal tract, particularly in genetically susceptible individuals.
Distinguishing Between IBS and IBD
While IBS and IBD share some similar symptoms, there are key differences that can help distinguish between the two conditions:
- IBS is a functional disorder characterized by gut-brain axis dysfunction, whereas IBD involves chronic inflammation and structural damage to the intestines.
- Diagnosis of IBS is based on symptoms and exclusion of other conditions, whereas diagnosis of IBD involves objective evidence of inflammation through tests such as endoscopy or imaging studies.
- Treatment approaches for IBS focus on symptom management and improving quality of life, while treatment for IBD targets inflammation and aims to prevent complications.
Conclusion
In summary, Irritable Bowel Syndrome (IBS) and Inflammatory Bowel Disease (IBD) are distinct gastrointestinal conditions with different underlying causes, mechanisms, and treatment approaches.
While they share some similarities in symptoms, understanding the key differences between IBS and IBD is essential for accurate diagnosis and appropriate management.
Individuals experiencing gastrointestinal symptoms should seek evaluation by a healthcare provider for proper diagnosis and guidance on treatment options tailored to their specific condition.
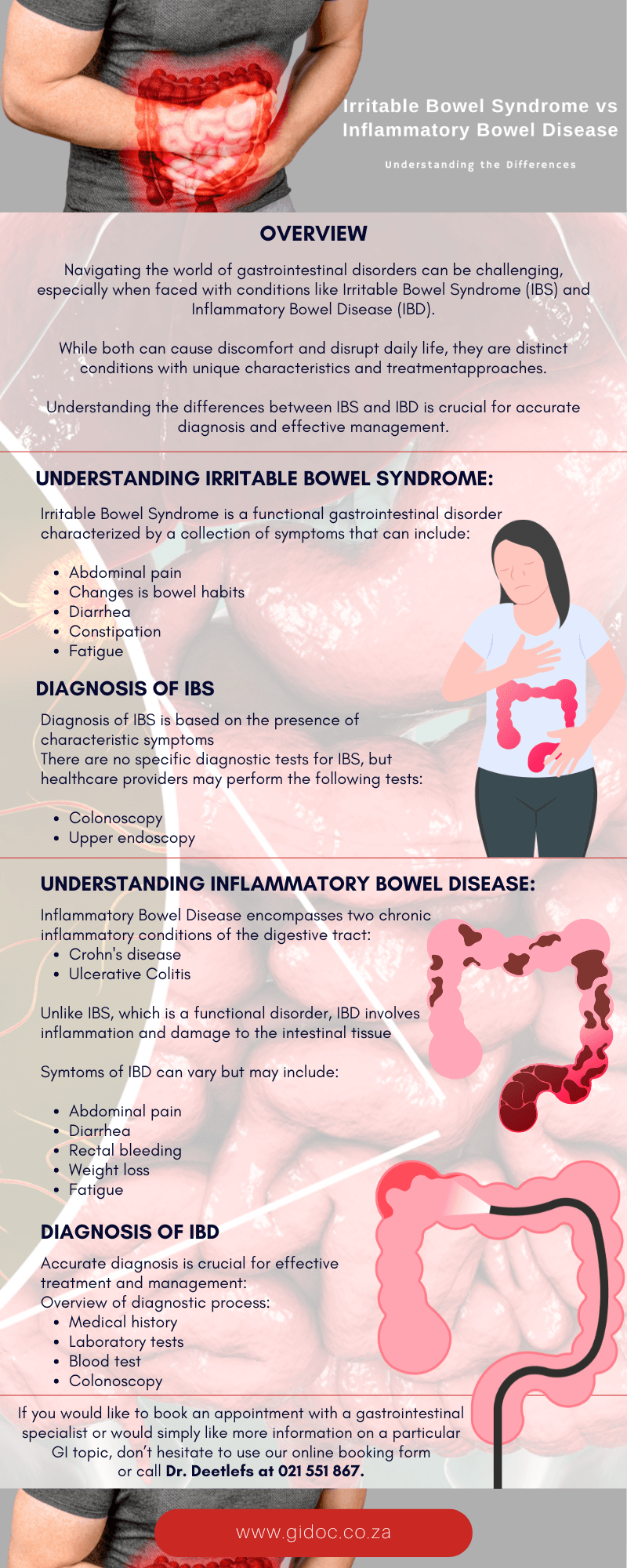
Contact Doctor Deetlefs
Gi Doc Capetown is a practice founded to provide medical solutions in the area of gastroenterology.
Over the years, Dr Eduan Deetlefs has earned the reputation of a trusted health expert providing consultative, diagnostic, and therapeutic endoscopic and related services to patients in
Cape Town and beyond.
If you would like to book an appointment with a gastrointestinal (GI) specialist or would simply like more information on a particular GI topic, don’t hesitate to use our online booking form or call Dr. Deetlefs at 021 551 867.
DISCLAIMER: PLEASE READ CAREFULLY
The information on this website is to provide general guidance. In no way does any of the information provided reflect definitive medical advice and self-diagnoses should not be made based on information obtained online. It is important to consult a Gastroenterologist or medical doctor regarding ANY and ALL symptoms or signs including, but not limited to: abdominal pain, haemorrhoids or anal / rectal bleeding as it may a sign of a serious illness or condition. A thorough consultation and examination should ALWAYS be performed for an accurate diagnosis and treatment plan. Be sure to call a physician or call our office today and schedule a consultation.
© Dr. Eduan Deetlefs, Registered Gastroenterologist, GI Doc Cape Town
Our website information is not intended or implied to be a substitute for professional medical advice, diagnosis or treatment. Please consult a doctor about your specific condition. Only a trained physician can determine an accurate diagnosis and proper treatment.