Do you know what your liver does and are you taking good care of it?
If not, this may be the time for you to start taking care of this part of your body that is responsible for digesting meals and eliminating toxins from the body.
In this article, we will discuss one of the common liver diseases known as cirrhosis.
Overview
The liver is a dark reddish-brown organ that weighs roughly 1.5kg.
The liver is involved in a variety of bodily functions, including protein synthesis and blood clotting, cholesterol, glucose (sugar), and iron metabolism.
Its primary function is to filter blood from the digestive tract before it is sent throughout the body.
Chemicals are detoxified and medicines are metabolized by the liver and secretes bile, which is then reabsorbed by the intestines.
This aids in the removal of waste materials from the liver. This important organ filters the blood that leaves the stomach and intestines.
What is Liver Cirrhosis
Liver cirrhosis is a disease in which the liver scars irreversibly.
It causes permanent damage because scar tissue obstructs your liver’s ability to function normally.
Cirrhosis is the final stage of the fibrosis (scarring) of the liver, which is caused by a variety of liver illnesses or diseases such as prolonged alcoholism or hepatitis.
When the liver is harmed by disease or excessive alcohol intake, it attempts to heal itself by forming scar tissue.
Scar tissues continue to grow as cirrhosis advances. Cirrhosis in its advanced stages can be fatal.
The scar tissue reduces the liver’s capacity to metabolize nutrients, hormones, medicines, and natural toxins by blocking blood flow through the liver (poisons). It also lowers the liver’s production of proteins and other chemicals.
Cirrhosis causes irreversible damage; however, it can be minimized to some extent if discovered early and treated effectively.

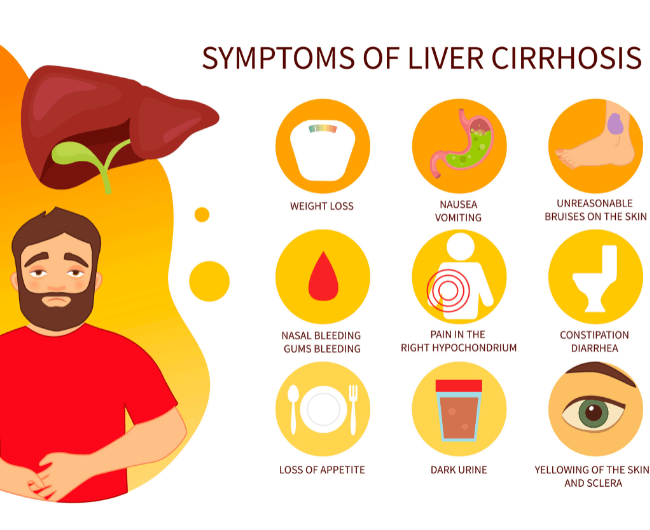
What are the Symptoms of Liver Cirrhosis?
It is possible that you will not experience any symptoms at an early stage.
However, when the damage to your liver worsens, you may notice problems like the following:
- Fatigue or exhaustion, feeling weak
- Prone to bleeding or bruising
- Swelling in abdomen
- Edema (swelling of abdomen and/or legs, feet, ankles)
- Weight loss and a lack of appetite
- Nausea
It is also possible that you will notice changes in your skin, such as:
- Jaundice (a condition wherein one’s skin and eyes turn yellow)
- Severe itching
- Blood vessels that look like spider webs
- Redness in the palms of your hands or nail bleaching
You may even have changes in your thinking, such as difficulties with focus or remembering.
Confusion, drowsiness, and slurred speech can also be symptoms of liver cirrhosis.
What are the Causes of Liver Cirrhosis?
Cirrhosis is always the result of a problem or disease with the liver. If you do not treat the underlying cause of your liver cirrhosis, it will worsen, and your healthy liver cells will eventually be unable to keep up.
In fact, you might start to feel the symptoms above. Your liver may even be unable to function properly or at all after some time.
It’s critical to figure out what’s causing this cirrhosis so you can get the appropriate treatment and prevent it from worsening. The following are the most typical causes:
- Serious alcohol abuse
- Hepatitis B, Hepatitis C, and Hepatitis D
- Nonalcoholic fatty liver disease (fat accumulating in the liver)
- Autoimmune hepatitis
- Chronic heart failure
- Ascites (a condition in which fluid accumulates in the abdominal cavity)
- Infections, including syphilis (a bacterial infection usually spread by sexual contact) and brucellosis (a bacterial infection that spreads from animals to people)
- Bad or allergic reactions to certain medications like methotrexate (chemotherapeutic drug that suppresses the immune system) and isoniazid (an antibiotic used for the treatment of tuberculosis)
Other causes could be hereditary such as:
- Wilson’s disease (copper accumulates in your liver, brain, and other key organs due to a rare congenital condition)
- Biliary atresia (blockage in the tubes or ducts that transport bile from the liver to the gallbladder)
- Cystic fibrosis (a condition that affects the lungs and digestive system wherein mucus or a thick sticky substance produced by the body can clog the lungs and impede the pancreas)
- Galactosemia or galactose in the blood (an illness that affect the body’s capacity to digest and produce energy from the sugar galactose)
- Alagille syndrome (a condition that affects the liver and other organs because of the presence of fewer tiny bile ducts in the liver causing scarring and damage to the organ)
- Alpha-1 antitrypsin deficiency or AAT deficiency (a disorder that increases your chances of developing lung and liver illness if AAT, proteins produced by the liver that protects the lungs, gets trapped in the liver)
Stages of Cirrhosis
There are different stages of cirrhosis depending on how well your liver is working.
Once you have been diagnosed with a liver cirrhosis, you will know what stage you are in, whether compensated or decompensated.
Stage 1.
You have compensated cirrhosis if you have cirrhosis but no visible symptoms (you are asymptomatic). Compensated cirrhosis occurs when the liver is scarred yet still capable of performing most of its essential functions.
Stage 2.
Liver cirrhosis is characterized by increasing portal hypertension (scarring of the liver) and the appearance of varices (veins that are enlarged or swollen).
Stage 3.
Decompensated cirrhosis is defined as cirrhosis that has progressed to the point where the liver is having difficulty functioning and you are experiencing symptoms of the disease.
Stage 4.
This stage can be fatal, and some persons acquire end-stage liver disease (ESLD), which is lethal without a transplant. 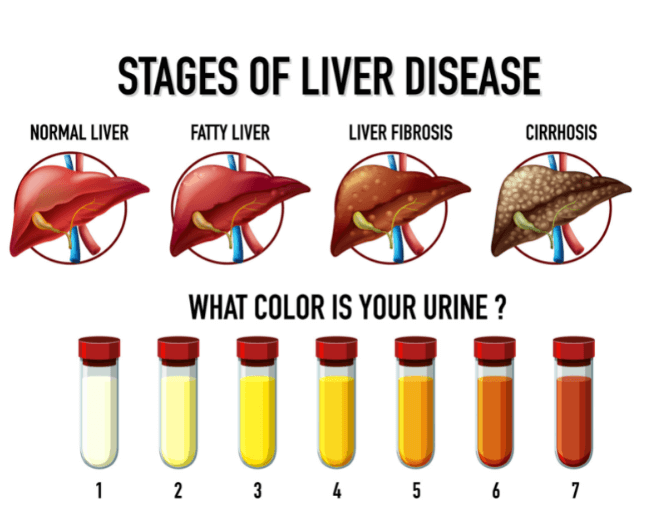
Preventive Measures against Liver Cirrhosis
The risk factors are the most typical causes mentioned above, serious alcohol abuse and viral hepatitis. Being overweight is also a problem.
Obesity raises the risk of nonalcoholic fatty liver disease and nonalcoholic steatohepatitis, both of which can develop to cirrhosis.
While there is no cure for cirrhosis because the damage done to your liver will be permanent, you can prevent liver cirrhosis or keep it from getting worse by taking the following preventive measures:
- Stop drinking alcoholic beverages (or limit it if you really cannot stop at once so you can later get used to none). You can even ask your doctor to suggest a treatment program for addiction.
- If you have chronic hepatitis (B or C), have it treated with antiviral medications.
- Avoid drugs and medications that can strain your liver and ask your doctor if it’s okay to take over-the-counter medicines like acetaminophen, aspirin, or ibuprofen because these are bad for ascites.
- If you are obese, lose weight. Your liver can be harmed by having too much body fat. If you are obese or overweight, talk to your doctor about a weight-loss strategy.
- Consume an adequate amount of protein. Have a healthy, well-balanced, and low-fat diet.
- Get flu, pneumonia, and hepatitis A and B vaccinations.
It is strongly advised that you visit a doctor as soon as you notice the symptoms.

Conclusion
Cirrhosis develops as a late-stage consequence of liver disease.
In the early stages of the condition, you may not experience any symptoms.
Alcohol misuse, hepatitis, and nonalcoholic fatty liver disease are all common causes.
Cirrhosis treatment is determined by the origin of the disease and the extent of the damage.
Remember that prevention is better than cure.
If you would like to book an appointment with a gastrointestinal (GI) specialist or would simply like more information on a particular GI topic, don’t hesitate to use our online booking form or call Dr. Deetlefs at 021 551 867.
DISCLAIMER: PLEASE READ CAREFULLY
The information on this website is to provide general guidance. In no way does any of the information provided reflect definitive medical advice and self-diagnoses should not be made based on information obtained online. It is important to consult a Gastroenterologist or medical doctor regarding ANY and ALL symptoms or signs including, but not limited to: abdominal pain, haemorrhoids or anal / rectal bleeding as it may a sign of a serious illness or condition. A thorough consultation and examination should ALWAYS be performed for an accurate diagnosis and treatment plan. Be sure to call a physician or call our office today and schedule a consultation.
© Dr. Eduan Deetlefs, Registered Gastroenterologist, GI Doc Cape Town
Our website information is not intended or implied to be a substitute for professional medical advice, diagnosis or treatment. Please consult a doctor about your specific condition. Only a trained physician can determine an accurate diagnosis and proper treatment.


