Colorectal cancer (CRC) is cancer that occurs in the colon or rectum, where abnormal growths called polyps form.
According to the World Cancer Research Fund, colorectal cancer is the third (3rd) most common histologically diagnosed cancers worldwide.
This ranking is also true in South African cancer cases among women, while it ranks as the
second (2nd) leading cause of cancer deaths among South African men, which, only has as little as 0.1% survival rate.
A routine colonoscopy screening might be just what you need to not join the statistics.

What is a Routine Colonoscopy Screening?
A colonoscopy is a procedure doctors conduct to screen for colorectal cancer and can also help diagnose unexplained changes in bowel habits and abdominal pain.
Even without symptoms, undergoing a routine colonoscopy can help your doctor locate polyps so they can be removed before turning into cancer.
It aids doctors to find colorectal cancer at an early stage when a patient’s survival rate is still at its highest.
As it is a visual exam, colonoscopy screening involves the use of a colonoscope and a proctosigmoidoscope to look at the entire length of the colon and rectum.
These instruments are thin fiber optic devices with a light and video camera that are attached to the tip of a flexible tube to search for polyps.
The devices are passed through the anal orifice into the rectum and further inside into the colon. Mild sedation and pain medication are usually administered in this procedure.
Also, sspecial instruments can be passed through the colonoscope to get a biopsy (sample) or remove any suspicious-looking growths such as polyps if needed.
How Often Do I Need to Undergo Colonoscopy Screening?
Everybody should undergo a complete colonoscopy screening by the time they reach the age of forty-five.
By this age, the overall risk of developing colorectal cancer increases and early detection is vital for effective treatment.
If you are forty-five (45) years old or older, with an average risk of CRC you may have to routinely undergo colonoscopy once every 10 years.
People at increased or high risk of colorectal cancer might need to start colorectal cancer screening before age 45, be screened more often, and/or get specific tests.
As shown in this table, some indicators increase a person’s risk of developing colorectal cancer, and a higher risk requires more frequent colonoscopy screening:
| INDICATORS | Average Risk of CRC | High Risk of CRC | ||
| Colonoscopy requirement | Colonoscopy requirement | |||
| Personal history of colorectal cancer or certain types of polyps | ✖ | every 10 yrs. | ✔ | Regular colonoscopy, 1 year after previous surgery |
| Family history of colorectal cancer | ✖ | every 10 yrs. | ✔ | Before reaching age 45 |
| Personal history of inflammatory bowel disease (ulcerative colitis or Crohn’s disease) | ✖ | every 10 yrs. | ✔ | Colonoscopy at least 8 years after being diagnosed with inflammatory bowel disease. Follow-up colonoscopies should be done every 1 to 3 years, depending on the person’s risk factors for colorectal cancer and the findings on the previous colonoscopy. |
|
Personal history of getting radiation to the abdomen (belly) or pelvic area to treat a prior cancer
|
✖ | every 10 yrs. | ✔ | Colonoscopy at an earlier age (depending on how old they were when they got the radiation); often begins 5 years after the radiation was given or at age 30, may need to be screened more often than normal (such as at least every 3 to 5 years). |
| With genetic disease | ✖ | every 10 yrs. | ✔ | Colonoscopy as early as teenage years |
Colonoscopy Routine Screening vs. Diagnostic Colonoscopy
Screening colonoscopy and diagnostic colonoscopy basically perform the same procedures and only differ in purpose and timing.
While screening colonoscopy is a preventive measure to screen patients for cancerous polyps when they reached a certain age or if they have a family history of colon cancer, diagnostic colonoscopy is more of a curative response.
Diagnostic colonoscopies are done when a patient already exhibits specific symptoms that may suggest colon cancer, such as persistent diarrhea or constipation; blood in the stool; persistent abdominal cramps, gas or pain; weakness or fatigue; unexplained weight loss; and that feeling of not being able to empty completely no matter how many bowel movements.
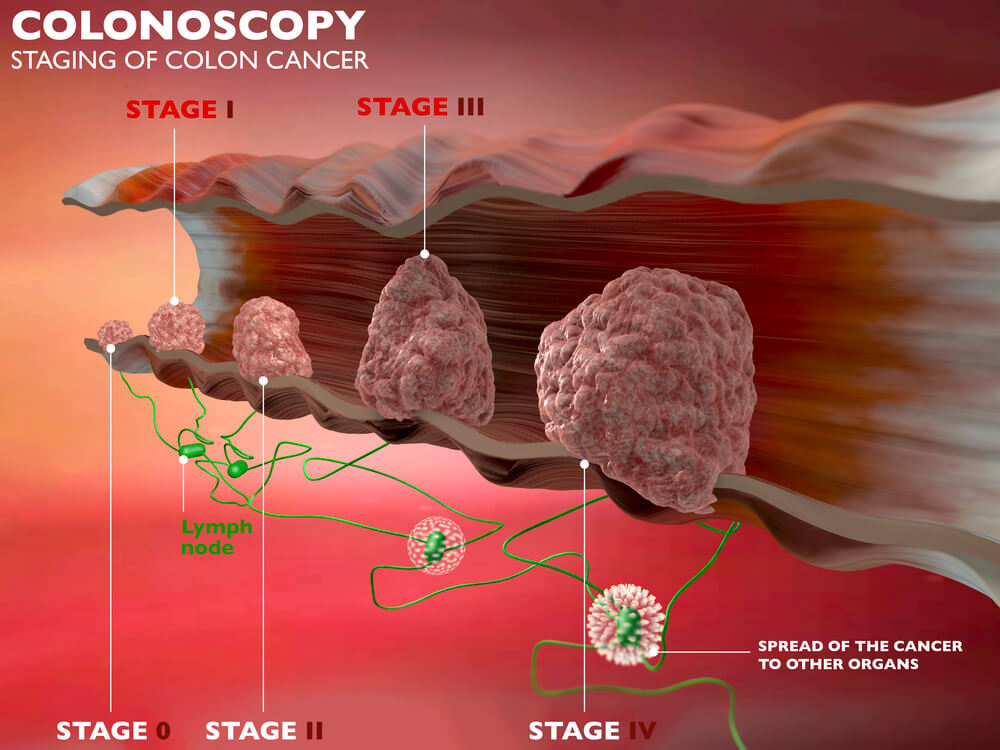
It is important to note that most colorectal cancer patients experience no symptoms in the early stages of the disease.
When symptoms start to show, cancer cells have most likely grown within the large intestine; therefore, it is important that you get screened.
Preparation: Things to Do to Prepare for a Colonoscopy
For your colonoscopy to be a success, you need to endure the hardship of purging as you need to empty your colon.
You will be prescribed a powerful bowel-clearing laxative resulting in frequent bowel movements or diarrhea both the night before or the morning of the procedure.
Failure to empty your colon may cause the polyps and lesions to be missed, the colonoscopy may take longer (increasing the risk of complications), or the whole process may need to be delayed and rescheduled – which means you will undergo another round of bowel prep (which you wouldn’t wish to).
Your doctor may ask you to refrain from ingesting solid food and only intake water the day before your procedure.
If you have pre-existing conditions like diabetes, heart problems, or high blood pressure, or if you have been on medication or supplements with iron, let your physician know at least a week before the screening.
Also inform your doctor if you have been taking aspirin, warfarin (Coumadin, Jantoven), anticoagulants like dabigatran (Pradaxa) or rivaroxaban (Xarelto). You might be asked to adjust your dosages or stop taking the medications temporarily.
During: What Happens During a Colonoscopy
The whole procedure typically lasts approximately 30-60 minutes and may take longer if the doctor sees abnormalities that need removal.
Many people are given medicines so they are put into a sleepy state where they can still converse but they won’t have any memory of the conversation.
You may still feel mild cramping during the procedure which you can reduce by taking several slow deep breaths. Some people, however, may need stronger anesthesia.
You will be asked to lie on your left side on the examining table as the doctor will insert the colonoscope through the rectum and advance to the other end of the large intestine while the instrument transmits images of the colon lining to the screen.
The scope is bendable so the doctor can move it around the curves of your colon. You may be asked to change position as needed to facilitate the moving of the scope.
Your colon expands as the scope blows air into your colon so the doctor can see more clearly.
When the doctor has finished, he will slowly withdraw the colonoscope while carefully examining the lining of your bowel.
Recovery: What to Do After a Colonoscopy
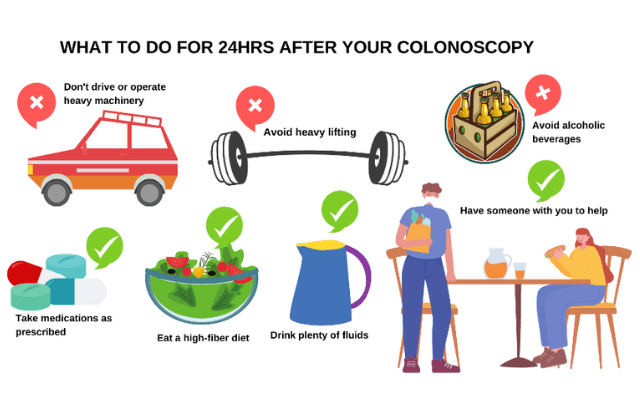
It is particularly important that you are accompanied by someone in the next 24 hours after your procedure.
As you have been sedated, it is not recommended that you drive, fly, or do any strenuous activity.
Watch your diet, drink plenty of fluids, and stick to your prescribed medications.
If polyps have been removed in your colon, you might need to take at least 7 days to rest and alter your activities including exercising
Possible Risks of Colonoscopy
Although rare, some complications may arise after a colonoscopy. Studies estimate the overall risk of complications for routine colonoscopy to be as low as 1.6%.
Perforation (a hole in the intestine), bleeding, post-polypectomy syndrome, reaction to anesthetic and infection are some of the possible complications that may occur.
Despite these, colonoscopy is an overall very safe test, and the benefits of undergoing routine colonoscopy screening far outweigh the discomfort and possible risks that may arise.
We highly recommend that you get screened because as the saying goes, “prevention is better than cure”.
DISCLAIMER: PLEASE READ CAREFULLY
The information on this website is to provide general guidance. In no way does any of the information provided reflect definitive medical advice and self-diagnoses should not be made based on information obtained online. It is important to consult a Gastroenterologist or medical doctor regarding ANY and ALL symptoms or signs including, but not limited to: abdominal pain, haemorrhoids or anal / rectal bleeding as it may a sign of a serious illness or condition. A thorough consultation and examination should ALWAYS be performed for an accurate diagnosis and treatment plan. Be sure to call a physician or call our office today and schedule a consultation.
© Dr. Eduan Deetlefs, Registered Gastroenterologist, GI Doc Cape Town
Our website information is not intended or implied to be a substitute for professional medical advice, diagnosis or treatment. Please consult a doctor about your specific condition. Only a trained physician can determine an accurate diagnosis and proper treatment.


