Liver Health: Prevention and Treatment of Non-Alcoholic Fatty Liver Disease (NAFLD)
Introduction
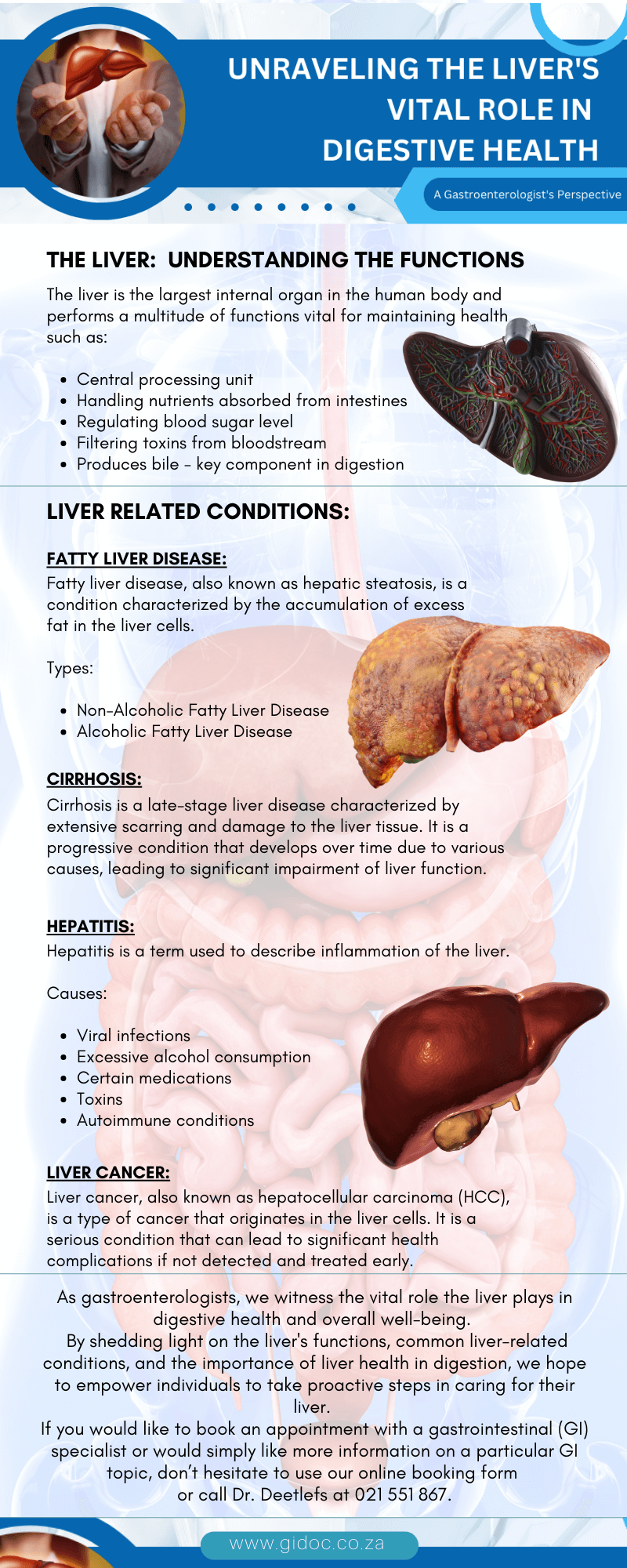
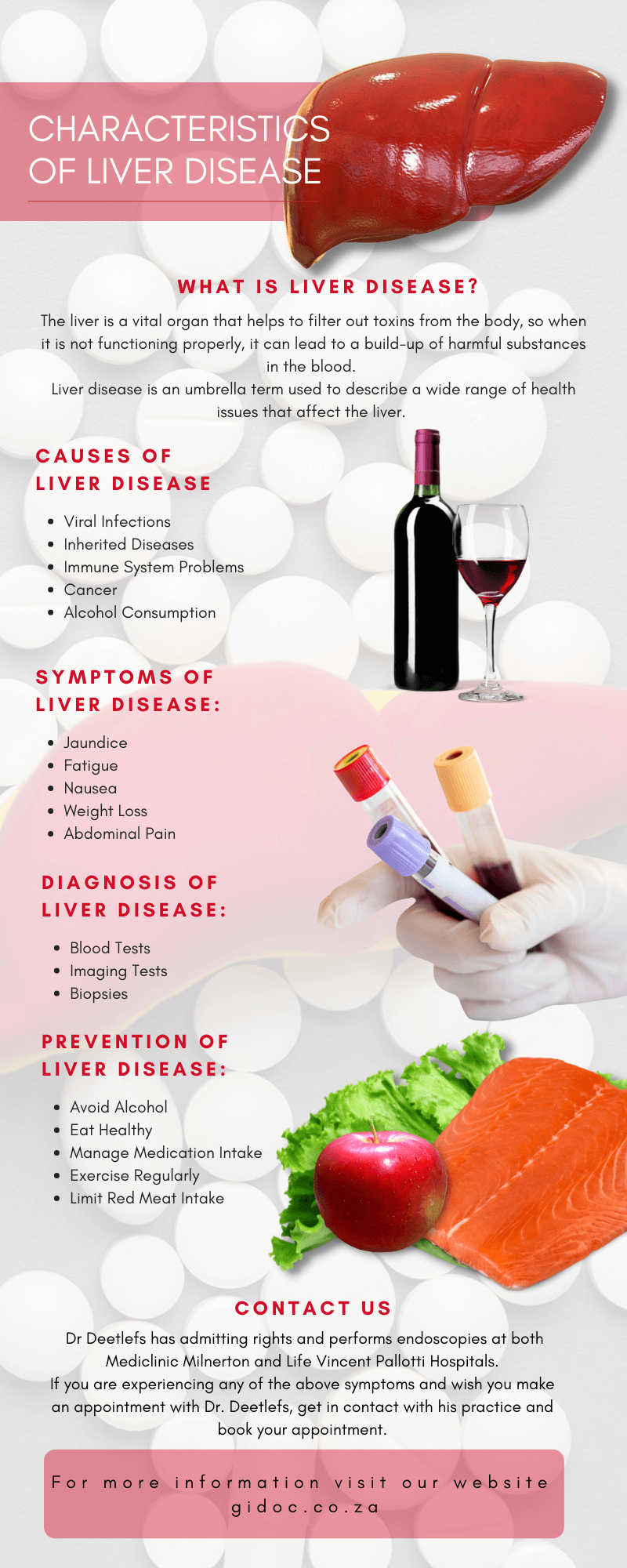
Non-Alcoholic Fatty Liver Disease (NAFLD) is a condition characterized by excessive fat accumulation in the liver in people who consume little to no alcohol.
It has emerged as one of the most common liver disorders worldwide, affecting an estimated 25% of the global population.
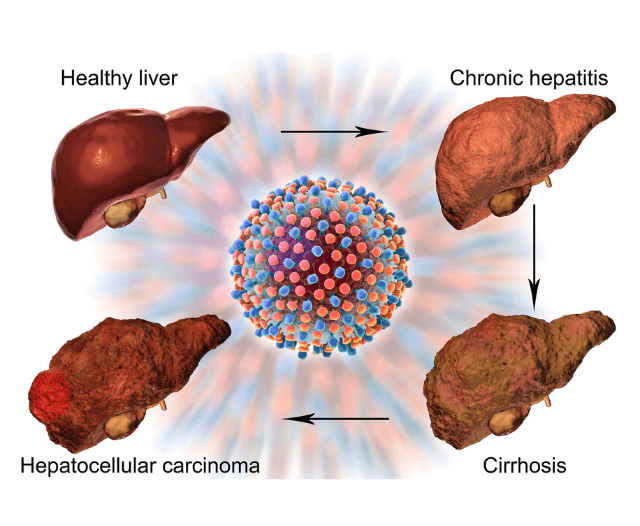
NAFLD can progress to more severe liver diseases, such as non-alcoholic steatohepatitis (NASH), cirrhosis, and liver cancer, if left unmanaged.
Understanding the prevention and treatment strategies for NAFLD is crucial for maintaining liver health and overall well-being.
Understanding NAFLD
NAFLD is often divided into two categories: simple fatty liver (steatosis) and non-alcoholic steatohepatitis (NASH).
While simple fatty liver is generally benign, NASH involves liver inflammation and damage, which can progress to more serious liver conditions.
Risk Factors for NAFLD
Several risk factors contribute to the development of NAFLD, including:
- Obesity: Excess body weight, particularly visceral fat, is a significant risk factor.
- Type 2 Diabetes: Insulin resistance and high blood sugar levels are strongly associated with NAFLD.
- Metabolic Syndrome: A cluster of conditions, including hypertension, dyslipidemia, and insulin resistance, increases the risk.
- Sedentary Lifestyle: Lack of physical activity contributes to obesity and metabolic abnormalities.
- Genetic Predisposition: Certain genetic variants can increase susceptibility to NAFLD.
- Poor Dietary Habits: High intake of saturated fats, refined sugars, and processed foods can lead to fat accumulation in the liver.
Prevention of NAFLD
Preventing NAFLD involves adopting a healthy lifestyle and addressing modifiable risk factors.
Here are some key strategies:
- Maintain a Healthy Weight
- Achieve and Maintain a Healthy BMI: Aim for a body mass index (BMI) within the healthy range (18.5-24.9).
- Gradual Weight Loss: Avoid rapid weight loss, as it can exacerbate liver inflammation. Aim for a gradual weight loss of 1-2 pounds per week.
- Adopt a Balanced Diet
- Mediterranean Diet: Emphasize whole grains, lean proteins, healthy fats (such as olive oil), and plenty of fruits and vegetables.
- Reduce Sugar Intake: Limit consumption of sugary beverages, desserts, and snacks. Opt for natural sweeteners like honey and fruit.
- Avoid Trans Fats: Minimize intake of trans fats found in processed and fried foods.
- Increase Fiber Intake: Incorporate fiber-rich foods like legumes, whole grains, and vegetables to improve digestion and reduce fat absorption.
- Regular Physical Activity
- Aerobic Exercise: Engage in at least 150 minutes of moderate-intensity aerobic exercise, such as brisk walking, swimming, or cycling, each week.
- Strength Training: Include resistance exercises at least two days per week to build muscle mass and improve metabolism.
- Stay Active: Incorporate more physical activity into daily routines, such as taking the stairs, walking during breaks, and reducing sedentary time.
- Monitor and Manage Health Conditions
- Control Blood Sugar Levels: If you have diabetes, monitor blood glucose levels and follow a diabetic-friendly diet.
- Manage Blood Pressure: Maintain a healthy blood pressure through lifestyle changes and, if necessary, medication.
- Regular Check-ups: Schedule regular check-ups with your healthcare provider to monitor liver health and other metabolic conditions.

Treatment of NAFLD
If you have been diagnosed with NAFLD, several treatment strategies can help manage the condition and prevent progression to more severe liver diseases.
- Lifestyle Modifications
- Weight Loss: Gradual weight loss through a combination of diet and exercise is the most effective way to reduce liver fat and inflammation.
- Healthy Diet: Follow a balanced diet that is low in saturated fats, refined sugars, and processed foods. Focus on nutrient-dense foods that support liver health.
- Regular Exercise: Engage in regular physical activity to improve insulin sensitivity, reduce liver fat, and enhance overall health.
- Medications
- Insulin Sensitizers: Medications such as metformin can improve insulin sensitivity and reduce liver fat in patients with NAFLD.
- Lipid-lowering Agents: Statins and other lipid-lowering medications may be prescribed to manage dyslipidemia and reduce cardiovascular risk.
- Vitamin E: Antioxidant therapy with vitamin E has shown promise in reducing liver inflammation in some patients with NASH.
- Medical Interventions
- Bariatric Surgery: For individuals with severe obesity and NAFLD, bariatric surgery may be considered to achieve significant and sustained weight loss.
- Liver Transplant: In cases of advanced liver disease or liver failure, a liver transplant may be necessary.
- Monitoring and Follow-up
- Regular Liver Function Tests: Periodic liver function tests can help monitor the progression of NAFLD and assess the effectiveness of treatment.
- Imaging Studies: Ultrasound, MRI, or CT scans may be used to evaluate liver fat content and detect any signs of liver damage.
- Liver Biopsy: In some cases, a liver biopsy may be performed to assess the extent of liver inflammation and fibrosis.

Support and Resources
Living with NAFLD can be challenging, but support and resources are available to help you manage the condition effectively.
- Healthcare Team
- Primary Care Physician: Your primary care physician can provide initial diagnosis, management, and referrals to specialists if needed.
- Hepatologist: A liver specialist (hepatologist) can offer advanced care and monitor liver health.
- Dietitian/Nutritionist: A registered dietitian or nutritionist can help create a personalized eating plan to support liver health and weight management.
- Fitness Trainer: A certified fitness trainer can develop an exercise program tailored to your needs and abilities.
- Support Groups
- Online Communities: Join online forums and social media groups for individuals with NAFLD to share experiences, tips, and support.
- Local Support Groups: Look for local support groups or organizations that offer in-person meetings and resources.
- Educational Resources
- Books and Publications: Read books and articles on liver health and NAFLD to stay informed and motivated.
- Websites and Apps: Use reputable websites and mobile apps to track your diet, exercise, and health progress.
The Importance of Regular Monitoring
Regular health check-ups and monitoring are crucial for individuals with NAFLD. Early detection of liver changes allows for timely intervention and better management of the condition.
Blood Tests
Liver Function Tests (LFTs): These tests measure enzymes and proteins in the blood that indicate liver health. Elevated levels can signal liver damage.
Fasting Blood Glucose and HbA1c: Monitoring blood sugar levels helps manage diabetes and prevent further liver damage.
Lipid Profile: Assessing cholesterol and triglyceride levels helps manage dyslipidemia, a common co-condition of NAFLD.
Imaging Studies
Ultrasound: A non-invasive method to detect liver fat and assess liver size.
MRI and CT Scans: These provide more detailed images of the liver and can help identify liver fat, inflammation, and fibrosis.
FibroScan: A specialized ultrasound that measures liver stiffness, indicating fibrosis and cirrhosis.
Liver Biopsy
Indications: Recommended when non-invasive tests suggest significant liver damage or when the diagnosis is uncertain.
Procedure: Involves taking a small tissue sample from the liver for microscopic examination to assess inflammation, fibrosis, and fat content.

Conclusion
Non-Alcoholic Fatty Liver Disease (NAFLD) is a prevalent liver condition that can lead to severe liver diseases if not managed properly.
Prevention and treatment of NAFLD primarily involve lifestyle modifications, such as maintaining a healthy weight, adopting a balanced diet, engaging in regular physical activity, and managing underlying health conditions.
For those diagnosed with NAFLD, a combination of lifestyle changes, medications, and medical interventions can help manage the condition and prevent progression.
By taking proactive steps to support liver health, individuals can reduce the risk of developing NAFLD and its associated complications.
Regular monitoring, support from healthcare professionals, and access to educational resources can empower individuals to make informed decisions and maintain a healthy liver for years to come.
Remember, a healthy liver is essential for overall well-being, and making small, sustainable changes today can have a significant impact on your future health.

Contact Dr. Deetlefs
Dr. Deetlefs has earned the reputation of a trusted health expert providing consultative, diagnostic, and therapeutic endoscopic and related services to patients in Cape Town and beyond.
DISCLAIMER: PLEASE READ CAREFULLY
The information on this website is to provide general guidance. In no way does any of the information provided reflect definitive medical advice and self-diagnoses should not be made based on information obtained online. It is important to consult a Gastroenterologist or medical doctor regarding ANY and ALL symptoms or signs including, but not limited to: abdominal pain, haemorrhoids or anal / rectal bleeding as it may a sign of a serious illness or condition. A thorough consultation and examination should ALWAYS be performed for an accurate diagnosis and treatment plan. Be sure to call a physician or call our office today and schedule a consultation.
© Dr. Eduan Deetlefs, Registered Gastroenterologist, GI Doc Cape Town
Our website information is not intended or implied to be a substitute for professional medical advice, diagnosis or treatment. Please consult a doctor about your specific condition. Only a trained physician can determine an accurate diagnosis and proper treatment.