Liver Disease: Causes, Symptoms, and Treatments
Overview
Liver disease is a broad term that describes any sort of damage that affects the liver.
The liver is a vital organ that helps to filter toxins out of the blood, so when it is not functioning properly, it can have serious consequences.
Liver disease can be caused by a number of things, including alcohol abuse, viral infections, and certain medications.
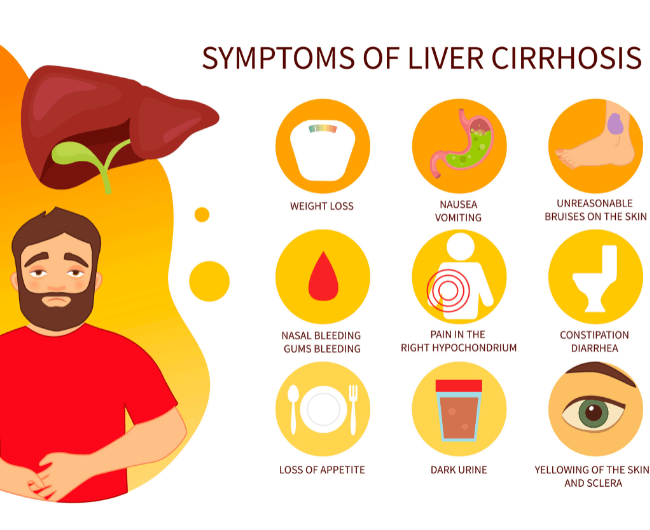
Symptoms of liver disease can include fatigue, nausea, and yellowing of the skin and eyes (jaundice).
If liver disease is caught early, it is often treatable with medication and lifestyle changes.
However, if the damage to the liver is severe, a transplant may be necessary.
In this article we discuss liver disease in depth, covering the causes, symptoms, and treatments thereof.
If you think you may have liver disease, it is important to see a doctor as soon as possible.
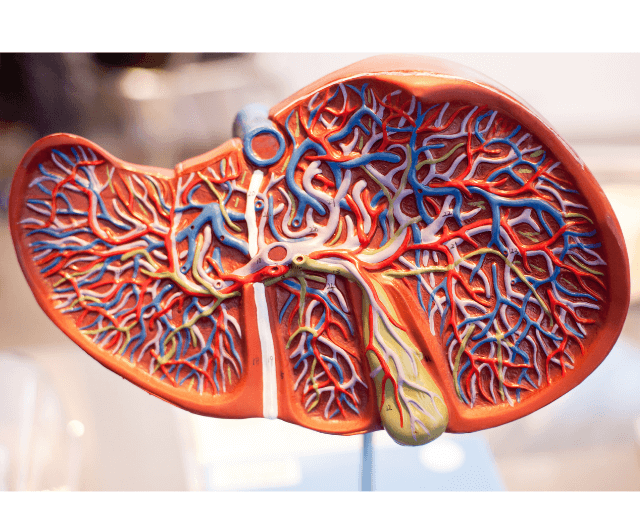
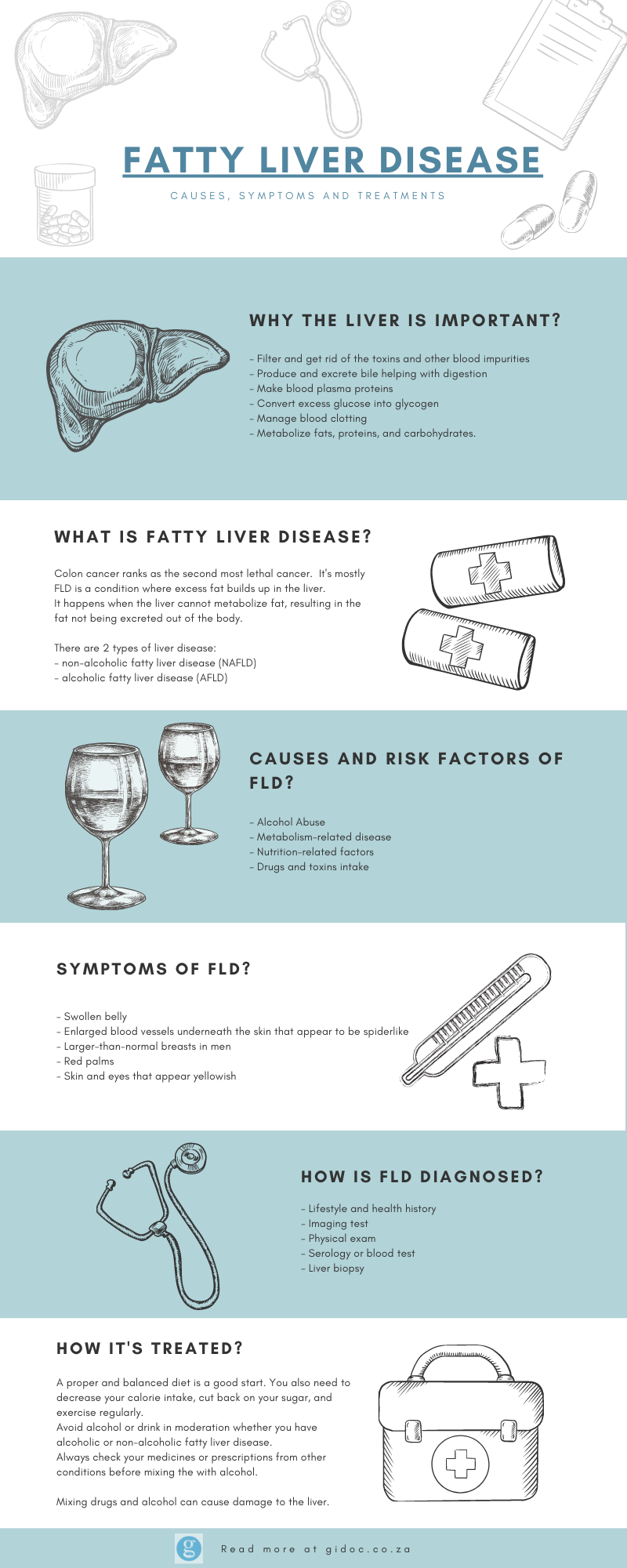
What Is the Function of The Liver?
The liver is one of your body’s most important organs and the second largest organ in the body.
Consisting of multiple lobes, it’s located just under your ribcage on the right side of your body.
The liver sits just to the left of your gallbladder, and its size is comparable to a football.
The liver has many functions, including filtering the blood, storing glycogen, and producing bile. The liver is also responsible for detoxifying the body and removing toxins from the blood.
The liver is a vital organ in the human body, so when it isn’t functioning properly, it can cause a number of problems.
What is Liver Disease?
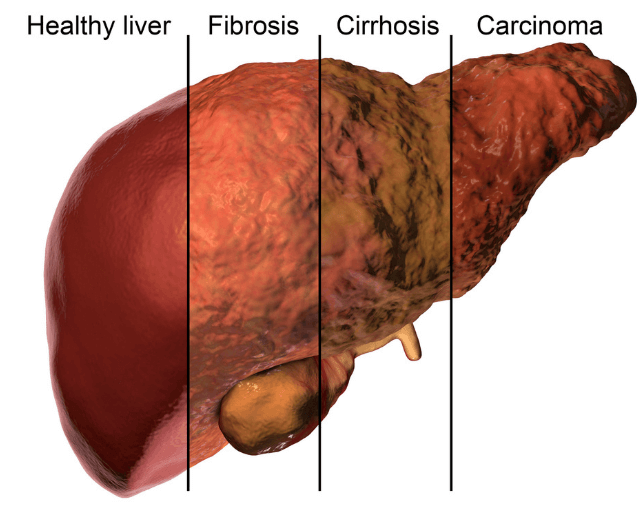
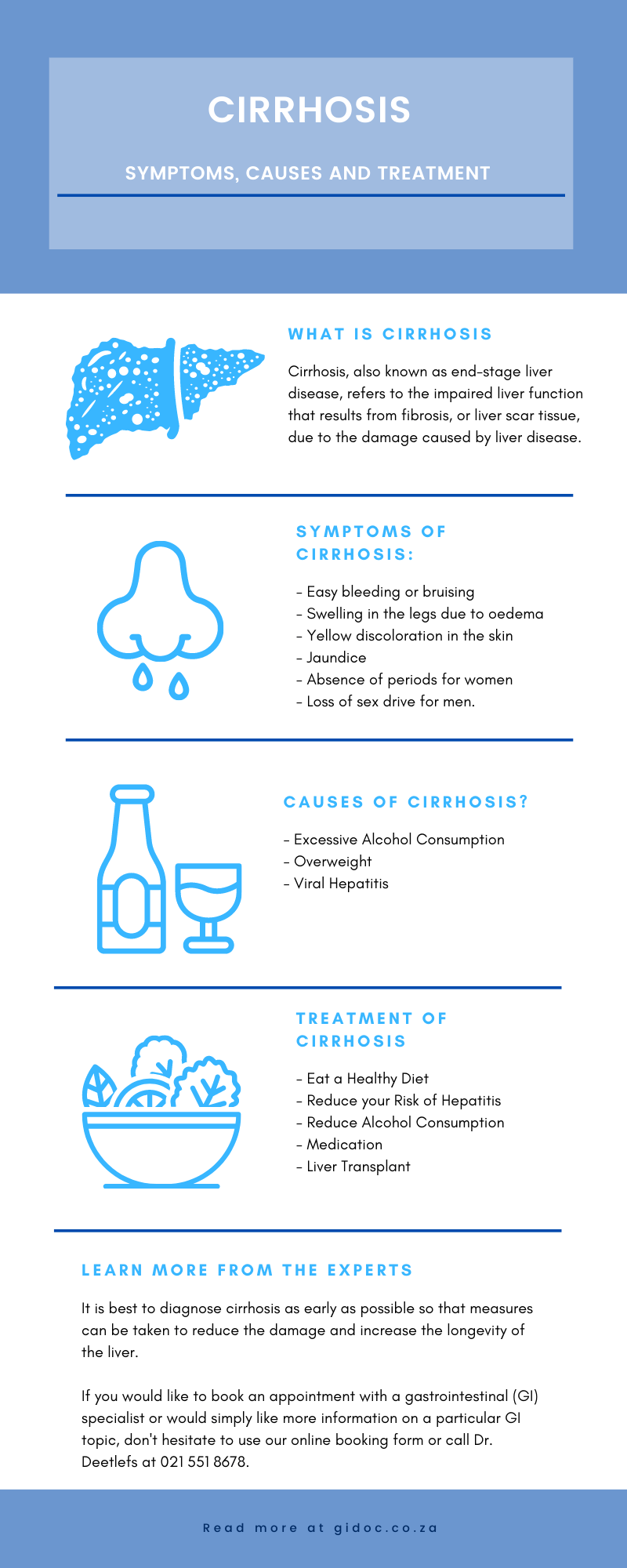
Liver disease is a general term for any type of damage that affects the liver.
It can be caused by a variety of things, including viruses, alcohol, and certain medications.
Liver disease can lead to a build-up of toxins in the body, which can cause a range of symptoms.
In severe cases, liver disease can be fatal. There is no one-size-fits-all approach to treatment, as it will depend on the underlying cause of the liver damage.
There are many different causes of liver disease, which we will discuss below.
Symptoms of Liver Disease
Liver disease is any disturbance of liver function that causes illness.
The liver is responsible for many vital functions within the body and when it is unable to perform these functions properly, it can result in a variety of symptoms that can be mild to severe.
There are many different causes of liver disease, ranging from viral infections to chronic alcohol abuse.
Symptoms of liver disease can include fatigue, weakness, weight loss, nausea and vomiting, yellowing of the skin and whites of the eyes (jaundice), itching, and easy bruising.
If you are experiencing any of these symptoms, it is important to see your doctor for a proper diagnosis.
Liver disease is often progressive and can be fatal if not treated properly.
Jaundice
Jaundice is a yellowing of the skin, mucous membranes, and the whites of the eyes. It is caused by an excess of bilirubin, a yellow pigment, in the blood.
Jaundice most commonly occurs when there is an obstruction in the bile ducts, preventing bile from draining from the liver.
This can lead to a build-up of bilirubin in the blood and a yellowing of the skin.
Swelling in the abdomen
If you have chronic liver disease, you may be aware of the many symptoms that come with the territory.
One symptom that is not as commonly discussed is abdominal swelling, or ascites.
This can be a very frustrating symptom, but there are treatments available to help.
There are a few different things that can cause ascites. One is portal hypertension. This is when the pressure in the portal vein, which goes from the intestines to the liver, is too high.
This can be caused by various things, such as liver scarring from hepatitis C.
Another cause of ascites is when the liver can’t make enough protein.
Fatigue
If you’re feeling tired all the time, it could be a sign that your liver is not functioning properly.
Liver disease can cause fatigue because the liver is not able to remove toxins from the body as efficiently as it should.
The build-up of toxins can lead to fatigue, muscle weakness, and other symptoms.
There are a number of different liver diseases that can cause fatigue. These include hepatitis, cirrhosis, and fatty liver disease.
If you have any of these conditions, it’s important to get treatment so that your liver can function properly, and you can feel your best.
Weight
As we all know, being overweight has many consequences including an increased risk for developing chronic diseases such as heart disease, stroke, and diabetes.
However, many people are unaware that being overweight also puts them at risk for developing liver disease.
Causes of Liver Disease
Liver disease can be caused by a number of things, including:
- Excessive alcohol consumption: Drinking more than the recommended amount of alcohol can damage the liver.
- Hepatitis: This is an inflammation of the liver that can be caused by a viral infection, such as the hepatitis C virus, or by autoimmune disease.
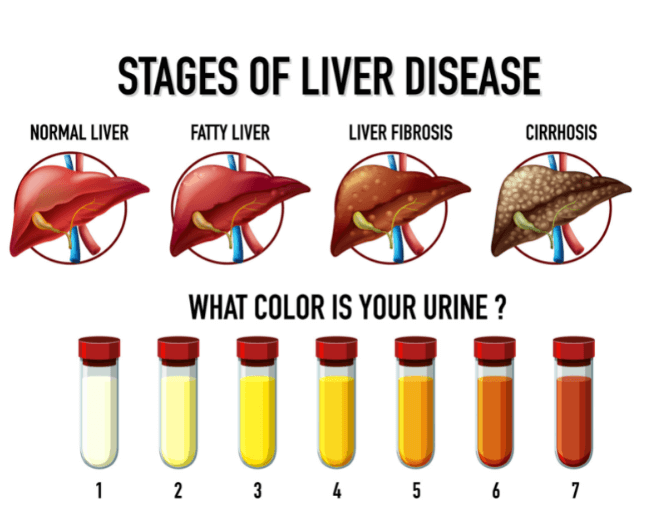
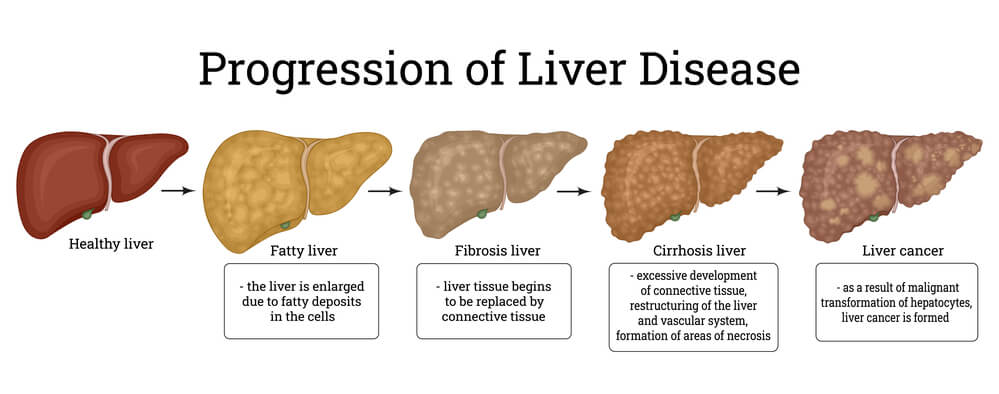
- Fatty liver: This occurs when there is an accumulation of fat in the liver. It can be caused by obesity, diabetes, or excessive alcohol.
- Alcohol Abuse: While there are many different types of liver disease, one of the most common is alcohol abuse. Alcohol abuse can cause a wide variety of problems, including liver damage, cirrhosis, and even cancer.
- Smoking: Few people know that smoking is one of the leading causes of liver disease. In fact, smoking is directly responsible for about 30% of all cases of liver disease. And, even if you don’t smoke, if you’re regularly exposed to secondhand smoke, you’re also at risk.
- Obesity: Obesity is a risk factor for many diseases, including liver disease. In fact, obesity is the leading cause of liver disease in the United States.
- Viruses: The most common types of liver disease are caused by viruses. Viruses are the leading cause of liver disease worldwide. In the United States, the most common viral causes of liver disease are hepatitis A, hepatitis B, and hepatitis C. Hepatitis A is a virus that is transmitted through contaminated food or water.
Diagnosis of Liver Disease
In order to diagnose liver disease, your doctor will likely take a complete medical history and perform a physical examination.
They may also order one or more of the following tests:
Liver function tests
These tests measure the levels of enzymes in your blood that are released by the liver.
Enzymes are proteins that help chemical reactions in the body.
Imaging Tests
These tests create pictures of the inside of your body. They may be used to look for a mass, tumor, or blockage in the liver.
Biopsy
This is a test in which a small sample of liver tissue is removed and examined for damage or disease.
Treatment of Liver Disease
If you have liver disease, it’s important to get early diagnosis and treatment.
Many types of liver disease can be treated successfully if they’re caught early.
There are many different types of liver disease, and the treatment depends on the specific diagnosis. In general, however, most liver diseases can be treated with a combination of medication and lifestyle changes.
Medications used to treat liver disease include antiviral drugs, antibiotics, antifungal drugs, and immunosuppressants.
These drugs can help slow the progression of liver damage, and they may also be used to manage the symptoms of liver disease.
Getting Help
In conclusion, it’s important to stay positive and prevent liver disease from developing.
Regardless of your diet, it’s good to be aware of what you’re eating and drinking.
Anything that encourages you to make better nutritional choices is worth considering.
Contact Dr. Deetlefs today to book your appointment online or call us on 021-5518678.
DISCLAIMER: PLEASE READ CAREFULLY
The information on this website is to provide general guidance. In no way does any of the information provided reflect definitive medical advice and self-diagnoses should not be made based on information obtained online. It is important to consult a Gastroenterologist or medical doctor regarding ANY and ALL symptoms or signs including, but not limited to: abdominal pain, haemorrhoids or anal / rectal bleeding as it may a sign of a serious illness or condition. A thorough consultation and examination should ALWAYS be performed for an accurate diagnosis and treatment plan. Be sure to call a physician or call our office today and schedule a consultation.
© Dr. Eduan Deetlefs, Registered Gastroenterologist, GI Doc Cape Town
Our website information is not intended or implied to be a substitute for professional medical advice, diagnosis or treatment. Please consult a doctor about your specific condition. Only a trained physician can determine an accurate diagnosis and proper treatment.