Irritable Bowel Syndrome (IBS) is a chronic functional gastrointestinal disorder that affects the large intestine.
It’s characterized by a cluster of symptoms, including abdominal pain, bloating, gas, diarrhea, constipation, or alternating between the two. While IBS doesn’t cause structural damage to the digestive tract, it significantly affects quality of life — both physically and mentally.
Emerging research shows a powerful link between the gut and the brain — commonly referred to as the gut-brain axis.
As a result, many individuals living with IBS not only suffer from gastrointestinal symptoms but also from mental health conditions such as anxiety and depression.
Fortunately, dietary modifications can play a powerful role in managing both physical symptoms and improving mental well-being.
This article provides a detailed look at dietary tips for managing IBS while exploring how the condition affects mental health and what you can do to improve both.
Understanding IBS and Its Triggers
IBS is a multifactorial condition, with no single identifiable cause. However, known triggers include:
- Certain foods (e.g., high-fat meals, dairy, caffeine)
- Stress and emotional changes
- Hormonal fluctuations
- Antibiotic use or gut infections
People with IBS may have hypersensitive guts, abnormal gut motility, and imbalances in the gut microbiota.
These factors can lead to irregular bowel habits and pain. Since there’s no cure for IBS, treatment focuses on symptom management, and diet is a primary strategy.
The Gut-Brain Axis: IBS and Mental Health
The gut and the brain are intricately connected via the gut-brain axis, a complex communication network involving the central nervous system, the enteric nervous system (which governs the GI tract), and the gut microbiome.
For individuals with IBS, this bidirectional link means:
- Stress and anxiety can trigger or worsen IBS symptoms.
- IBS flare-ups can lead to increased emotional distress, which may result in depression or social withdrawal.
- Many people with IBS report that their symptoms interfere with daily activities, work, relationships, and sleep, all of which impact mental health.
Addressing both the physical and psychological aspects of IBS is crucial for long-term management.
Dietary Tips for Managing IBS
Dietary changes are often the first step in managing IBS symptoms. However, because triggers vary widely from person to person, there is no one-size-fits-all diet.
Here are the most effective dietary strategies:
1. Adopt a Low-FODMAP Diet
FODMAPs are fermentable oligosaccharides, disaccharides, monosaccharides, and polyols — short-chain carbohydrates poorly absorbed in the small intestine. When fermented by gut bacteria, they produce gas and draw water into the bowel, leading to bloating, diarrhea, and discomfort.
High-FODMAP foods to avoid:
- Onions and garlic
- Apples, pears, and watermelon
- Wheat, barley, and rye
- Dairy (due to lactose)
- Legumes (beans, lentils, chickpeas)
- Artificial sweeteners (sorbitol, xylitol)
Low-FODMAP foods to include:
- Carrots, zucchini, spinach
- Berries, citrus fruits, bananas
- Gluten-free grains (rice, oats, quinoa)
- Lactose-free dairy or plant-based alternatives
- Eggs, chicken, tofu
A low-FODMAP diet involves three phases:
- Elimination of high-FODMAP foods
- Gradual reintroduction
- Personalization based on tolerance
Note: It’s best to follow this diet under the guidance of a registered dietitian.
2. Increase Soluble Fiber Intake
Fiber affects bowel movements and gut health, but not all fiber is equal. Insoluble fiber can aggravate symptoms, especially in people with diarrhea-predominant IBS. Soluble fiber, on the other hand, helps regulate bowel movements and reduce bloating.
Good sources of soluble fiber:
- Oats
- Psyllium husk
- Carrots
- Bananas
- Chia seeds
Start slow and increase fiber gradually to avoid triggering bloating or gas. Hydration is also essential — aim for at least 1.5 to 2 liters of water daily.
3. Avoid Common Irritants
Certain foods and beverages tend to aggravate IBS symptoms. Common culprits include:
- Caffeine: Stimulates the intestines and can worsen diarrhea.
- Alcohol: Can irritate the gut lining and alter motility.
- Fried and fatty foods: Harder to digest and often cause cramping.
- Spicy foods: May trigger pain or urgency in some individuals.
- Carbonated beverages: Introduce excess gas and cause bloating.
A food and symptom journal can help identify your specific triggers.
4. Eat Regular Meals and Avoid Overeating
Large meals can overwhelm the digestive system and cause cramping or bloating. Instead, opt for:
- Smaller, frequent meals throughout the day
- Eating slowly and chewing thoroughly
- Avoiding late-night eating or lying down immediately after meals
5. Consider Probiotics and Gut Health Supplements
Probiotics — beneficial bacteria — can help restore balance in the gut microbiome. Certain strains (e.g., Bifidobacterium infantis or Lactobacillus plantarum) have shown benefits for IBS symptoms, especially bloating and bowel irregularity.
Prebiotics (which feed good gut bacteria) and digestive enzymes may also support digestion, but responses vary. Consult a healthcare professional before starting supplements.

The Mental Health Impact of IBS
The mental burden of IBS is significant and often underestimated. Studies show that:
- Up to 60% of people with IBS also experience anxiety or depression.
- Chronic pain and unpredictability of bowel habits contribute to social withdrawal and isolation.
- IBS can impair work productivity, school attendance, and sexual health.
It’s important to acknowledge these challenges as part of the condition, not as a secondary issue. Treating IBS holistically includes supporting emotional well-being.
Psychological Strategies That Support Digestive Health
Given the gut-brain connection, managing stress and emotional health is vital in IBS treatment. Consider the following strategies:
1. Cognitive Behavioral Therapy (CBT)
CBT is a structured, evidence-based form of talk therapy that helps individuals identify and change negative thought patterns. It has proven highly effective for reducing IBS symptoms and anxiety.
2. Mindfulness and Relaxation Techniques
Practices such as meditation, deep breathing, and progressive muscle relaxation can reduce the stress response, calm the digestive system, and improve symptom control.
3. Exercise Regularly
Moderate physical activity — such as walking, swimming, or yoga — has multiple benefits:
- Improves mood and reduces anxiety
- Enhances digestion and reduces constipation
- Lowers inflammation
Aim for at least 30 minutes of activity most days of the week.
4. Sleep Hygiene
Poor sleep quality is linked to increased IBS symptom severity. Establish a consistent sleep schedule, limit screen time before bed, and create a calming nighttime routine.
Combining Diet and Mental Health Approaches
An integrative approach offers the best chance of success for managing IBS. Here’s a sample daily strategy:
- Morning: Start with a low-FODMAP breakfast (e.g., oatmeal with blueberries and chia seeds), followed by light stretching or a short walk.
- Afternoon: Practice mindfulness for 10 minutes. Eat a balanced lunch with lean protein and steamed veggies.
- Evening: Prepare a small dinner with easy-to-digest ingredients. Avoid caffeine and alcohol. Journal your symptoms and emotions before bed.
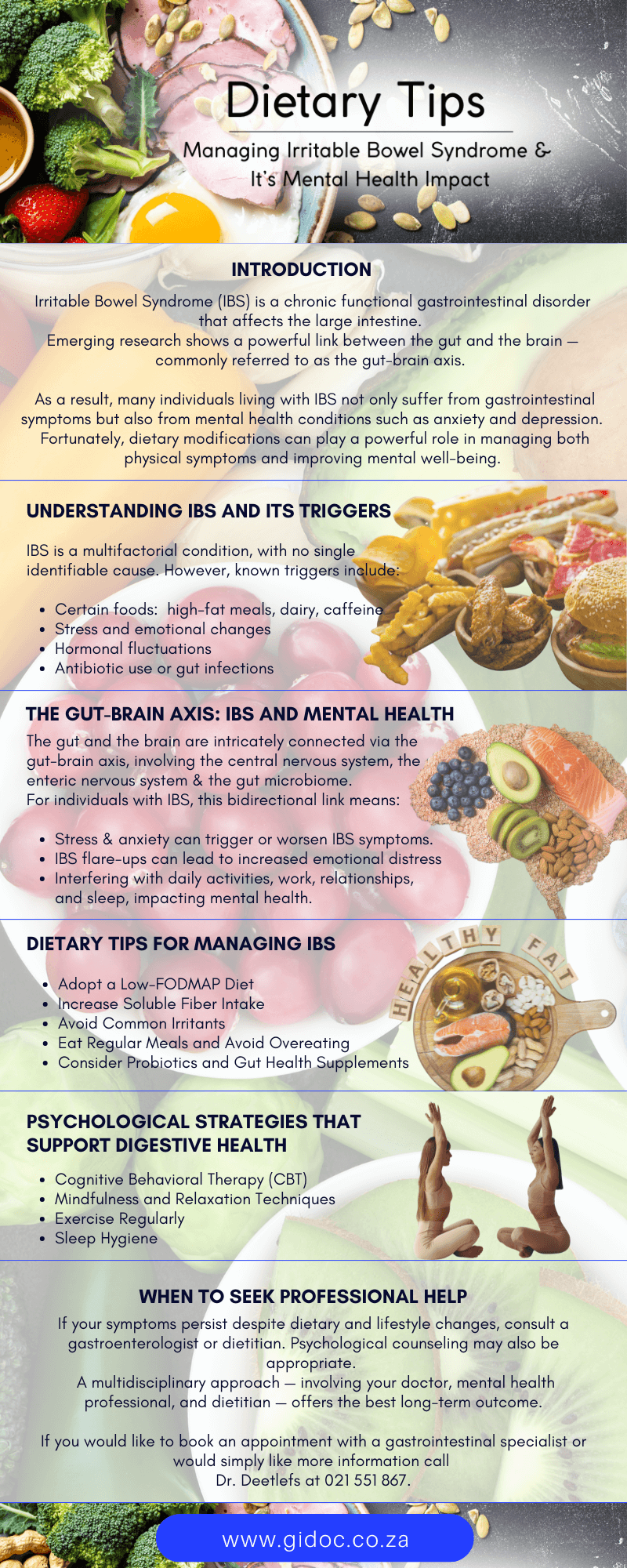
When to Seek Professional Help
If your symptoms persist despite dietary and lifestyle changes, consult a gastroenterologist or dietitian. Psychological counseling may also be appropriate.
A multidisciplinary approach — involving your doctor, mental health professional, and dietitian — offers the best long-term outcome.
Final Thoughts
Living with IBS can be frustrating and exhausting, both physically and mentally. But with the right dietary strategies and emotional support, you can take control of your symptoms and improve your quality of life.
A tailored, patient-centered approach that addresses both the digestive and psychological dimensions of IBS is the key to long-term relief.
Need Expert Digestive Care?
Dr. Deetlefs has earned the reputation of a trusted health expert providing consultative, diagnostic, and therapeutic endoscopic and related services to patients in Cape Town and beyond.
Dr. Deetlefs can be contacted to confirm the estimated breakdown should you be interested in having the procedure done.
DISCLAIMER: PLEASE READ CAREFULLY
The information on this website is to provide general guidance. In no way does any of the information provided reflect definitive medical advice and self-diagnoses should not be made based on information obtained online. It is important to consult a Gastroenterologist or medical doctor regarding ANY and ALL symptoms or signs including, but not limited to: abdominal pain, haemorrhoids or anal / rectal bleeding as it may a sign of a serious illness or condition. A thorough consultation and examination should ALWAYS be performed for an accurate diagnosis and treatment plan. Be sure to call a physician or call our office today and schedule a consultation.
© Dr. Eduan Deetlefs, Registered Gastroenterologist, GI Doc Cape Town
Our website information is not intended or implied to be a substitute for professional medical advice, diagnosis or treatment. Please consult a doctor about your specific condition. Only a trained physician can determine an accurate diagnosis and proper treatment.