Introduction
Irritable Bowel Syndrome (IBS) affects millions of people worldwide, causing significant discomfort and disruption to their daily lives.
This comprehensive guide aims to provide an in-depth understanding of IBS, including its symptoms, causes, and available treatment options.
By shedding light on this common gastrointestinal disorder, we hope to empower individuals to better manage their condition and seek appropriate medical care.
Definition and Prevalence:
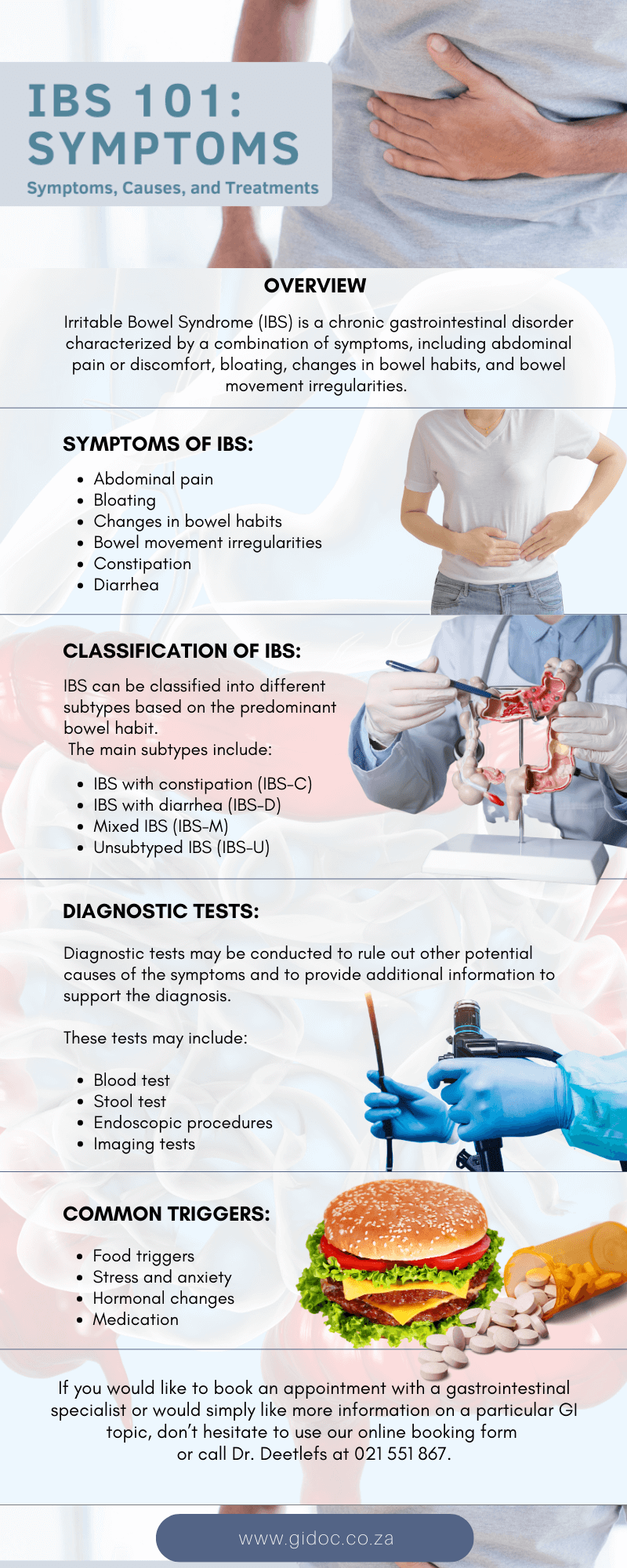
Irritable Bowel Syndrome (IBS) is a chronic gastrointestinal disorder characterized by a combination of symptoms, including abdominal pain or discomfort, bloating, changes in bowel habits, and bowel movement irregularities.
It is considered a functional disorder, meaning there are no structural abnormalities in the digestive system that can explain the symptoms.
Instead, IBS is believed to result from a dysregulation of the gut-brain axis, where the communication between the brain and the gut becomes disrupted.
IBS is a prevalent condition worldwide. Estimates suggest that around 10-15% of the global population is affected by IBS, making it one of the most common gastrointestinal disorders.
It can occur at any age, but it is most commonly diagnosed in individuals under the age of 50.
Women are more frequently affected than men, with a female-to-male ratio of approximately 2:1.
Classification of IBS Subtypes:
IBS can be classified into different subtypes based on the predominant bowel habit. These subtypes help to categorize the varying symptoms experienced by individuals with IBS.
The main subtypes include:
IBS with constipation (IBS-C):
Individuals with IBS-C experience infrequent and hard bowel movements. They may also have a feeling of incomplete evacuation after passing stool.
IBS with diarrhea (IBS-D):
Individuals with IBS-D experience frequent and loose bowel movements. They may have an urgent need to use the restroom and may also experience episodes of fecal incontinence.
Mixed IBS (IBS-M):
This subtype is characterized by alternating episodes of constipation and diarrhea. Individuals with IBS-M may experience varying bowel habits over time.
Unsubtyped IBS (IBS-U):
When the predominant bowel habit cannot be clearly identified, it is classified as IBS-U. In this subtype, individuals may have a combination of symptoms without a clear pattern.
Diagnostic Tests:
Diagnostic tests may be conducted to rule out other potential causes of the symptoms and to provide additional information to support the diagnosis. These tests may include:
Blood tests: These tests can help assess for signs of inflammation, anemia, or other underlying conditions.
Stool tests: Stool samples may be analyzed to rule out infections, parasites, or signs of gastrointestinal bleeding.
Endoscopic procedures: In some cases, an endoscopy or colonoscopy may be performed to visualize the gastrointestinal tract and rule out structural abnormalities or other conditions.
Imaging studies: Imaging tests, such as abdominal ultrasound or CT scan, may be ordered to evaluate the digestive organs and identify any abnormalities.
Common Triggers and Exacerbating Factors
While the exact cause of IBS is not fully understood, there are several triggers and exacerbating factors that can contribute to symptom flare-ups. These factors can vary from person to person, but some common triggers include:
Food triggers:
Certain foods and beverages can trigger IBS symptoms. Common triggers include spicy foods, fatty foods, caffeine, alcohol, and artificial sweeteners. It is important for individuals with IBS to identify their specific trigger foods through a process of elimination and personal observation.
Stress and anxiety:
Emotional factors, such as stress, anxiety, and depression, can significantly impact IBS symptoms. Stress can worsen gastrointestinal motility and sensitivity, leading to increased symptom severity.
Hormonal changes:
Hormonal fluctuations, particularly in women during their menstrual cycle, can influence IBS symptoms. Many women with IBS report changes in symptom severity during certain phases of their menstrual cycle.
Medications:
Certain medications, such as antibiotics, nonsteroidal anti-inflammatory drugs (NSAIDs), and some antidepressants, may worsen IBS symptoms.
Risk Factors and Demographics:
While IBS can affect anyone, several risk factors and demographics have been associated with an increased likelihood of developing the condition.
These include:
Age:
IBS can occur at any age, but it is commonly diagnosed in individuals under the age of 50. Symptoms often begin during adolescence or early adulthood.
Gender:
Women are more commonly affected by IBS than men. The reasons for this gender disparity are not entirely clear, but hormonal factors and differences in pain perception between genders may play a role.
Family history:
There is evidence to suggest that IBS may have a genetic component. Individuals with a family history of IBS are at a higher risk of developing the condition themselves.
Psychological factors:
Psychological conditions, such as anxiety and depression, are more common in individuals with IBS. Stressful life events, trauma, and a history of abuse may also increase the risk of developing IBS.
Understanding the symptoms, triggers, and risk factors associated with IBS is crucial in managing the condition effectively.
It is important for individuals with IBS to work closely with healthcare professionals to develop an individualized treatment plan that addresses their specific needs and triggers. By identifying and managing these factors, individuals can minimize symptom flare-ups and improve their overall quality of life.
Lifestyle Changes for IBS
Lifestyle modifications
- Dietary changes
- Stress management techniques
- Regular exercise
- Sleep hygiene B. Medications
- Antispasmodics
- Antidiarrheal agents
- Laxatives
- Probiotics
- Low-dose tricyclic antidepressants C. Psychological therapies
- Cognitive-behavioural therapy (CBT)
- Gut-directed hypnotherapy D. Complementary and alternative therapies
- Herbal remedies
- Acupuncture
Treatment options for IBS aim to alleviate symptoms, improve quality of life, and help individuals manage their condition effectively.
Treatment of IBS:
Lifestyle Modifications:
- Dietary Changes: Modifying the diet can be beneficial for many individuals with IBS. This may involve identifying and avoiding trigger foods, such as those high in fat, caffeine, or artificial sweeteners. Some individuals find relief by following specific diets, such as a low FODMAP (fermentable oligosaccharides, disaccharides, monosaccharides, and polyols) diet, which restricts certain carbohydrates that may worsen symptoms. Consulting a registered dietitian can provide personalized guidance.
- Stress Management Techniques: Stress and anxiety can exacerbate IBS symptoms. Engaging in stress management techniques, such as deep breathing exercises, meditation, yoga, or mindfulness practices, can help individuals reduce stress and improve symptom control.
- Regular Exercise: Physical activity has been shown to improve overall well-being and may help manage IBS symptoms. Engaging in regular exercise, such as walking, swimming, or cycling, can promote healthy digestion and reduce stress.
- Sleep Hygiene: Adequate sleep is essential for overall health and can positively impact IBS symptoms. Practicing good sleep hygiene, such as maintaining a regular sleep schedule, creating a comfortable sleep environment, and avoiding stimulating activities before bedtime, can promote restful sleep.
Medications
- Antispasmodics: These medications help relieve abdominal pain and cramping by relaxing the muscles in the intestines. They can be taken before meals to reduce symptoms during digestion.
- Antidiarrheal Agents: For individuals with IBS-D, antidiarrheal medications may be prescribed to control loose bowel movements and reduce urgency.
- Laxatives: In cases of IBS-C, laxatives can be used to relieve constipation and promote regular bowel movements. However, it is important to use them under medical supervision to avoid dependency.
- Probiotics: Probiotics are beneficial bacteria that can help restore a healthy balance in the gut. They may provide relief for some individuals with IBS by improving gut flora and reducing symptoms.
- Low-Dose Tricyclic Antidepressants: These medications are used in low doses to help manage pain and improve overall well-being. They can be particularly helpful for individuals with IBS who experience abdominal pain.
It is important for individuals with IBS to work closely with healthcare professionals to develop a personalized treatment plan. Not all treatments may be suitable for everyone, and the effectiveness of treatments can vary from person to person.
Conclusion
Dr. Deetlefs has earned the reputation of a trusted health expert providing consultative, diagnostic, and therapeutic endoscopic and related services to patients in Cape Town and beyond.
Dr Eduan prides himself on his ability to help his patients to the best of his ability by embracing good listening skills, effective communication, compassion and knowledge and skill honed during years of private gastroenterology practice.
If you would like to book an appointment with a gastrointestinal (GI) specialist or would simply like more information on a particular GI topic, don’t hesitate to use our online booking form
or call Dr. Deetlefs at 021 551 867.
DISCLAIMER: PLEASE READ CAREFULLY
The information on this website is to provide general guidance. In no way does any of the information provided reflect definitive medical advice and self-diagnoses should not be made based on information obtained online. It is important to consult a Gastroenterologist or medical doctor regarding ANY and ALL symptoms or signs including, but not limited to: abdominal pain, haemorrhoids or anal / rectal bleeding as it may a sign of a serious illness or condition. A thorough consultation and examination should ALWAYS be performed for an accurate diagnosis and treatment plan. Be sure to call a physician or call our office today and schedule a consultation.
© Dr. Eduan Deetlefs, Registered Gastroenterologist, GI Doc Cape Town
Our website information is not intended or implied to be a substitute for professional medical advice, diagnosis or treatment. Please consult a doctor about your specific condition. Only a trained physician can determine an accurate diagnosis and proper treatment.