Introduction
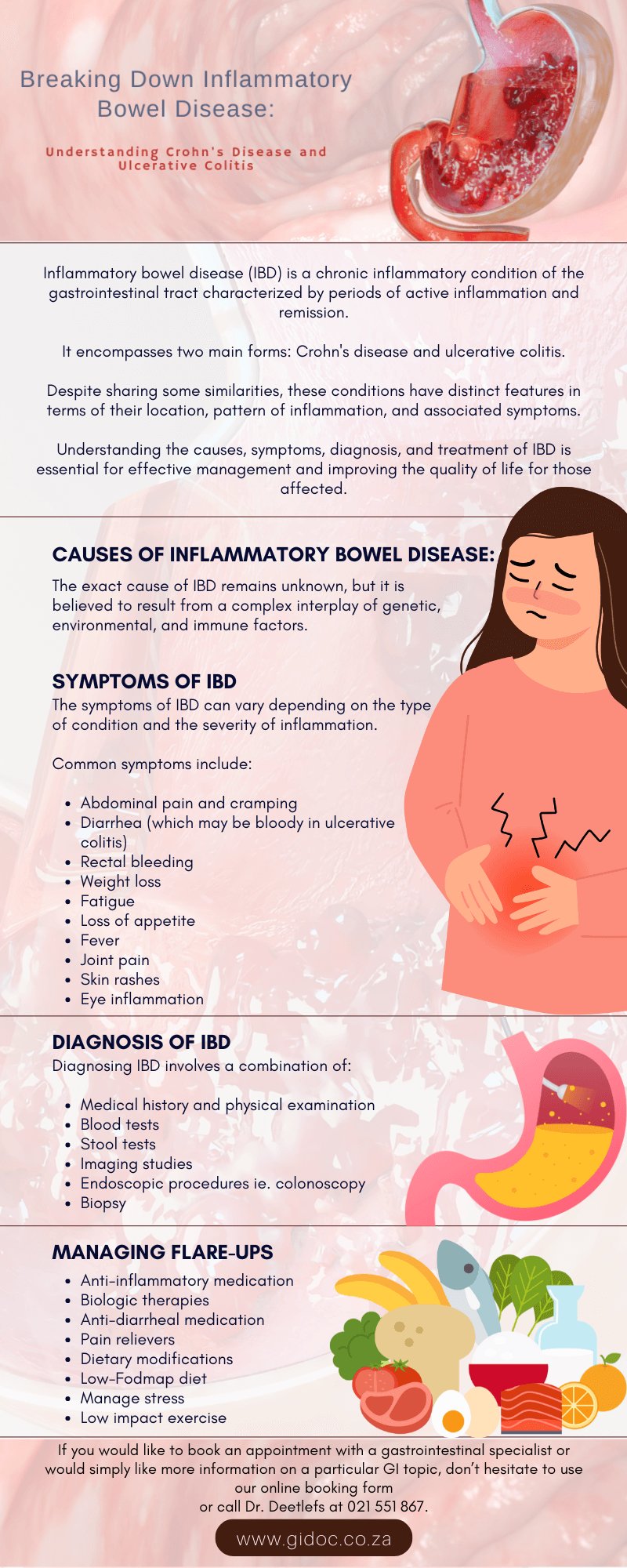
Inflammatory bowel disease (IBD) is a chronic inflammatory condition of the gastrointestinal tract characterized by periods of active inflammation and remission.
It encompasses two main forms: Crohn’s disease and ulcerative colitis.
Despite sharing some similarities, these conditions have distinct features in terms of their location, pattern of inflammation, and associated symptoms.
Understanding the causes, symptoms, diagnosis, and treatment of IBD is essential for effective management and improving the quality of life for those affected.
Causes of Inflammatory Bowel Disease
The exact cause of IBD remains unknown, but it is believed to result from a complex interplay of genetic, environmental, and immune factors.
Genetic predisposition plays a significant role, as individuals with a family history of IBD are at higher risk.
Environmental factors such as diet, smoking, stress, and microbial exposures may also contribute to the development of IBD.
Dysregulation of the immune system leads to chronic inflammation in the gastrointestinal tract, triggering the symptoms associated with IBD.
Symptoms of Inflammatory Bowel Disease
The symptoms of IBD can vary depending on the type of condition and the severity of inflammation.
Common symptoms include:
- Abdominal pain and cramping
- Diarrhea (which may be bloody in ulcerative colitis)
- Rectal bleeding
- Weight loss
- Fatigue
- Loss of appetite
- Fever
- Joint pain
- Skin rashes
- Eye inflammation
These symptoms can range from mild to severe and may fluctuate over time, with periods of active disease (flare-ups) alternating with periods of remission.

Diagnosis of Inflammatory Bowel Disease
Diagnosing IBD involves a combination of clinical evaluation, laboratory tests, imaging studies, and endoscopic procedures. The following diagnostic approaches may be utilized:
- Medical History and Physical Examination: A healthcare provider will review the patient’s medical history and perform a physical examination to assess symptoms and signs of IBD.
- Blood Tests: Blood tests may be conducted to assess inflammation (e.g., C-reactive protein, erythrocyte sedimentation rate), nutritional deficiencies, and markers associated with IBD (e.g., antibodies).
- Stool Tests: Stool samples may be analyzed for signs of infection, inflammation, or blood.
- Imaging Studies: Imaging tests such as X-rays, computed tomography (CT) scans, magnetic resonance imaging (MRI), or ultrasound may be used to visualize the gastrointestinal tract and assess for signs of inflammation or complications.
- Endoscopic Procedures: Colonoscopy and flexible sigmoidoscopy allow direct visualization of the colon and rectum, enabling the healthcare provider to assess inflammation, take tissue samples (biopsies), and exclude other conditions.
- Biopsy: Tissue samples obtained during endoscopic procedures are examined under a microscope to confirm the presence of inflammation and distinguish between Crohn’s disease and ulcerative colitis.
Colonoscopy Explained
A colonoscopy is a minimally invasive medical procedure used to examine the lining of the large intestine (colon) and rectum.
During the procedure, a thin, flexible tube with a tiny camera at the end (colonoscope) is inserted into the rectum and guided through the colon.
This allows the healthcare provider to visualize the entire length of the colon and identify any abnormalities, such as polyps, ulcers, inflammation, or signs of colorectal cancer.
Colonoscopy is considered the gold standard for colorectal cancer screening and can also help diagnose and treat various gastrointestinal conditions, including inflammatory bowel disease (IBD) and diverticulosis.
One of the primary benefits of colonoscopy is its ability to detect colorectal cancer at an early stage when it is most treatable and may even prevent cancer by removing precancerous polyps during the procedure.
Additionally, colonoscopy can provide valuable information for diagnosing and managing other gastrointestinal disorders, leading to better health outcomes for patients.
Despite the potential discomfort associated with preparation and the procedure itself, the benefits of colonoscopy in terms of early detection, prevention, and treatment of colorectal conditions far outweigh any temporary discomfort.
Regular screening colonoscopies are recommended for individuals at average risk of colorectal cancer starting at age 50 and at earlier ages for those with certain risk factors or family history.

Treatment of Inflammatory Bowel Disease
The goals of treatment for IBD are to reduce inflammation, control symptoms, induce and maintain remission, and improve the quality of life. Treatment strategies may include:
- Medications:
– Anti-inflammatory drugs (e.g., 5-aminosalicylates, corticosteroids)
– Immunomodulators (e.g., azathioprine, methotrexate)
– Biologic therapies (e.g., tumor necrosis factor-alpha inhibitors)
– Antibiotics (for specific complications or infections)
- Nutritional Therapy: Dietary modifications or nutritional supplementation may be recommended to address specific nutritional deficiencies or alleviate symptoms.
- Lifestyle Changes: Managing stress, getting regular exercise, staying hydrated, and avoiding tobacco use may help reduce symptoms and improve overall well-being.
- Surgery: In cases of severe disease or complications (e.g., intestinal obstruction, perforation, dysplasia, cancer), surgical intervention may be necessary to remove diseased portions of the intestine or alleviate symptoms.
Managing IBD Flare-ups
Managing flare-ups of inflammatory bowel disease (IBD) involves a multifaceted approach aimed at reducing inflammation, alleviating symptoms, and promoting healing of the gastrointestinal tract.
One key aspect of managing flare-ups is medication therapy, which may include anti-inflammatory drugs such as corticosteroids, 5-aminosalicylates, and immunomodulators to help control inflammation and induce remission.
Biologic therapies, which target specific molecules involved in the inflammatory response, may also be prescribed for moderate to severe flare-ups.
Additionally, symptom management strategies such as anti-diarrheal medications, pain relievers, and dietary modifications can help alleviate symptoms like diarrhea, abdominal pain, and cramping.
Patients may be advised to follow a low-residue or low-FODMAP diet to reduce bowel irritation and avoid triggering foods such as spicy or high-fiber foods. Maintaining adequate hydration, getting enough rest, and managing stress through relaxation techniques or counseling can also play a crucial role in managing flare-ups.
In some cases, hospitalization may be necessary for severe flare-ups or complications such as dehydration, severe pain, or intestinal obstruction. During hospitalization, patients may receive intravenous fluids, nutritional support, and more intensive medical therapy.
It’s important for individuals with IBD to work closely with their healthcare providers to develop a personalized management plan tailored to their specific needs and circumstances, with the goal of achieving symptom control, preventing complications, and improving quality of life.
Regular monitoring and follow-up care are essential for adjusting treatment as needed and optimizing long-term outcomes.

Conclusion:
Inflammatory bowel disease is a chronic condition characterized by inflammation of the gastrointestinal tract, which can significantly impact a person’s quality of life.
While the exact cause of IBD remains unknown, a combination of genetic, environmental, and immune factors is believed to contribute to its development.
Early diagnosis and appropriate treatment are essential for managing symptoms, preventing complications, and improving long-term outcomes for individuals with IBD.
With proper medical care, lifestyle modifications, and ongoing support, many people with IBD can achieve symptom control and lead fulfilling lives.
If you suspect you may have IBD or are experiencing symptoms suggestive of the condition, consult with a healthcare provider for evaluation, diagnosis, and personalized treatment recommendations.
Contact Doctor Deetlefs
Gi Doc Capetown is a practice founded to provide medical solutions in the area of gastroenterology.
Over the years, Dr Eduan Deetlefs has earned the reputation of a trusted health expert providing consultative, diagnostic, and therapeutic endoscopic and related services to patients in
Cape Town and beyond.
If you would like to book an appointment with a gastrointestinal (GI) specialist or would simply like more information on a particular GI topic, don’t hesitate to use our online booking form or call Dr. Deetlefs at 021 551 867.
DISCLAIMER: PLEASE READ CAREFULLY
The information on this website is to provide general guidance. In no way does any of the information provided reflect definitive medical advice and self-diagnoses should not be made based on information obtained online. It is important to consult a Gastroenterologist or medical doctor regarding ANY and ALL symptoms or signs including, but not limited to: abdominal pain, haemorrhoids or anal / rectal bleeding as it may a sign of a serious illness or condition. A thorough consultation and examination should ALWAYS be performed for an accurate diagnosis and treatment plan. Be sure to call a physician or call our office today and schedule a consultation.
© Dr. Eduan Deetlefs, Registered Gastroenterologist, GI Doc Cape Town
Our website information is not intended or implied to be a substitute for professional medical advice, diagnosis or treatment. Please consult a doctor about your specific condition. Only a trained physician can determine an accurate diagnosis and proper treatment.


