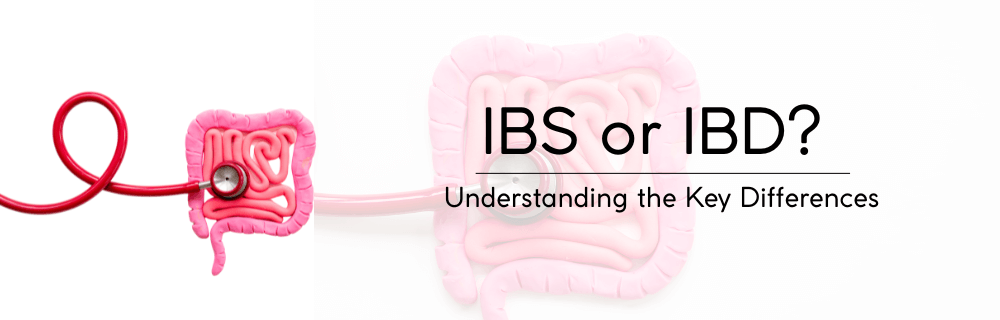
IBS or IBD? Understanding the Key Differences
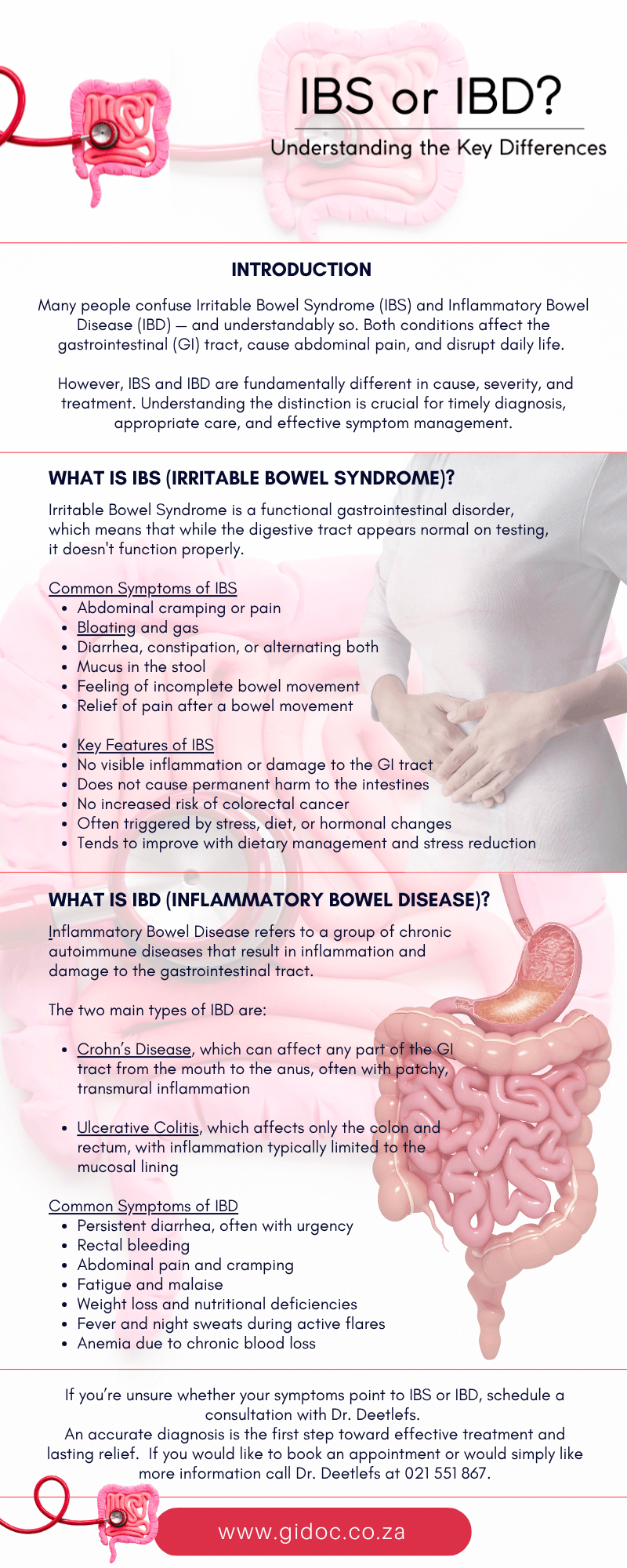
Many people confuse Irritable Bowel Syndrome (IBS) and Inflammatory Bowel Disease (IBD) — and understandably so. Both conditions affect the gastrointestinal (GI) tract, cause abdominal pain, and disrupt daily life.
However, IBS and IBD are fundamentally different in cause, severity, and treatment. Understanding the distinction is crucial for timely diagnosis, appropriate care, and effective symptom management.
In this article, we’ll explore the key differences between IBS and IBD, outline common symptoms, delve into diagnosis and treatment approaches, and offer guidance for patients living with either condition.
What Is IBS (Irritable Bowel Syndrome)?
Irritable Bowel Syndrome is a functional gastrointestinal disorder, which means that while the digestive tract appears normal on testing, it doesn’t function properly.
IBS affects the large intestine (colon) and is characterized by chronic abdominal discomfort, bloating, and altered bowel habits. Though it does not cause inflammation or damage to the bowel tissue, its symptoms can be severe and significantly affect quality of life.
IBS is believed to be caused by a complex interplay between the brain and gut, often referred to as the gut-brain axis. Abnormal muscle contractions in the intestine, heightened pain sensitivity, and changes in gut bacteria may all contribute to the development of IBS.
Common Symptoms of IBS
- Abdominal cramping or pain
- Bloating and gas
- Diarrhea (IBS-D), constipation (IBS-C), or alternating both (IBS-M)
- Mucus in the stool
- Feeling of incomplete bowel movement
- Relief of pain after a bowel movement
Key Features of IBS
- No visible inflammation or damage to the GI tract
- Does not cause permanent harm to the intestines
- No increased risk of colorectal cancer
- Often triggered by stress, diet, or hormonal changes
- Tends to improve with dietary management and stress reduction

What Is IBD (Inflammatory Bowel Disease)?
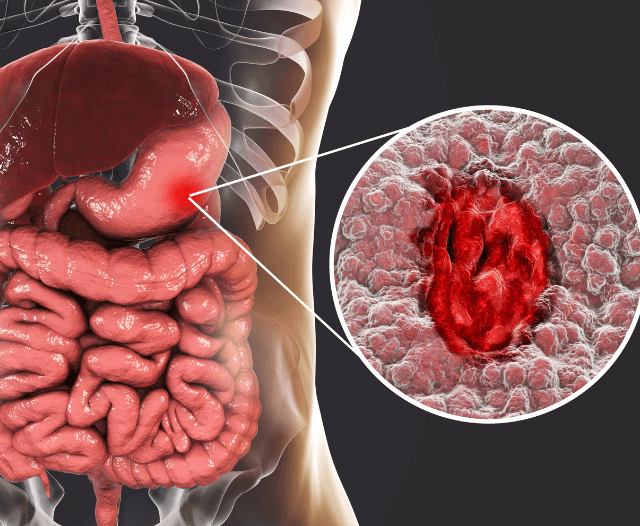
Inflammatory Bowel Disease refers to a group of chronic autoimmune diseases that result in inflammation and damage to the gastrointestinal tract. The two main types of IBD are:
- Crohn’s Disease, which can affect any part of the GI tract from the mouth to the anus, often with patchy, transmural inflammation
- Ulcerative Colitis, which affects only the colon and rectum, with inflammation typically limited to the mucosal lining
IBD is an autoimmune condition where the body mistakenly attacks healthy cells in the GI tract, leading to inflammation, ulceration, and complications over time. Unlike IBS, IBD can cause serious structural damage to the bowel and may require intensive medical treatment or surgery.
Common Symptoms of IBD
- Persistent diarrhea, often with urgency
- Rectal bleeding
- Abdominal pain and cramping
- Fatigue and malaise
- Weight loss and nutritional deficiencies
- Fever and night sweats during active flares
- Anemia due to chronic blood loss
Extraintestinal Manifestations
IBD can also affect other parts of the body beyond the digestive tract:
- Joint pain or arthritis
- Skin disorders like erythema nodosum
- Eye inflammation (uveitis)
- Liver disorders such as primary sclerosing cholangitis
Key Features of IBD
- Visible inflammation, ulcers, and damage to the GI tract
- Can lead to complications like strictures, fistulas, abscesses, and increased cancer risk
- Requires long-term medical treatment, and sometimes surgery
- May involve periods of remission and flare-ups
IBS vs IBD: A Side-by-Side Comparison
| Feature | IBS | IBD |
| Nature of Condition | Functional disorder | Autoimmune/inflammatory disease |
| Damage to GI Tract | None | Inflammation and structural damage |
| Risk of Colon Cancer | No | Increased risk (especially in UC) |
| Bleeding | Rare | Common |
| Diagnosis | Based on symptoms and exclusion | Confirmed by colonoscopy and biopsy |
| Treatment Goals | Symptom relief | Inflammation control and disease remission |
| Medications | Antispasmodics, fiber, laxatives | Biologics, immunosuppressants, steroids |
| Surgery Required | Rare | Often needed in severe cases |
| Mental Health Impact | Common, stress-related | Anxiety and depression due to disease burden |
Causes and Risk Factors
IBS Causes and Risk Factors
- Gut-brain axis dysfunction
- Stress and anxiety
- Dietary triggers (e.g., FODMAPs, caffeine, spicy foods)
- Hormonal fluctuations (more common in women)
- Post-infectious IBS after gastroenteritis
- Genetic and early life factors
IBD Causes and Risk Factors
- Immune system dysfunction
- Genetic predisposition (family history of IBD)
- Environmental triggers (e.g., antibiotics, pollution, Western diet)
- Smoking (increases Crohn’s risk, but may be protective in UC)
- Alterations in gut microbiota
- Urban living and lower vitamin D levels

Diagnosis: IBS vs. IBD
How Is IBS Diagnosed?
IBS is typically diagnosed after ruling out more serious conditions. Physicians may:
- Use the Rome IV criteria (abdominal pain related to defecation, lasting at least 1 day per week over 3 months)
- Review a detailed symptom and diet history
- Order blood tests to rule out anemia, celiac disease, or infection
- Use stool tests to rule out inflammation (e.g., fecal calprotectin)
- Conduct colonoscopy if red-flag symptoms are present
How Is IBD Diagnosed?
IBD diagnosis involves more advanced testing to confirm inflammation:
- Blood tests for CRP, ESR, and iron levels
- Stool tests like fecal calprotectin and occult blood
- Colonoscopy with tissue biopsy to assess extent and severity
- MRI or CT enterography to view the small bowel in Crohn’s disease
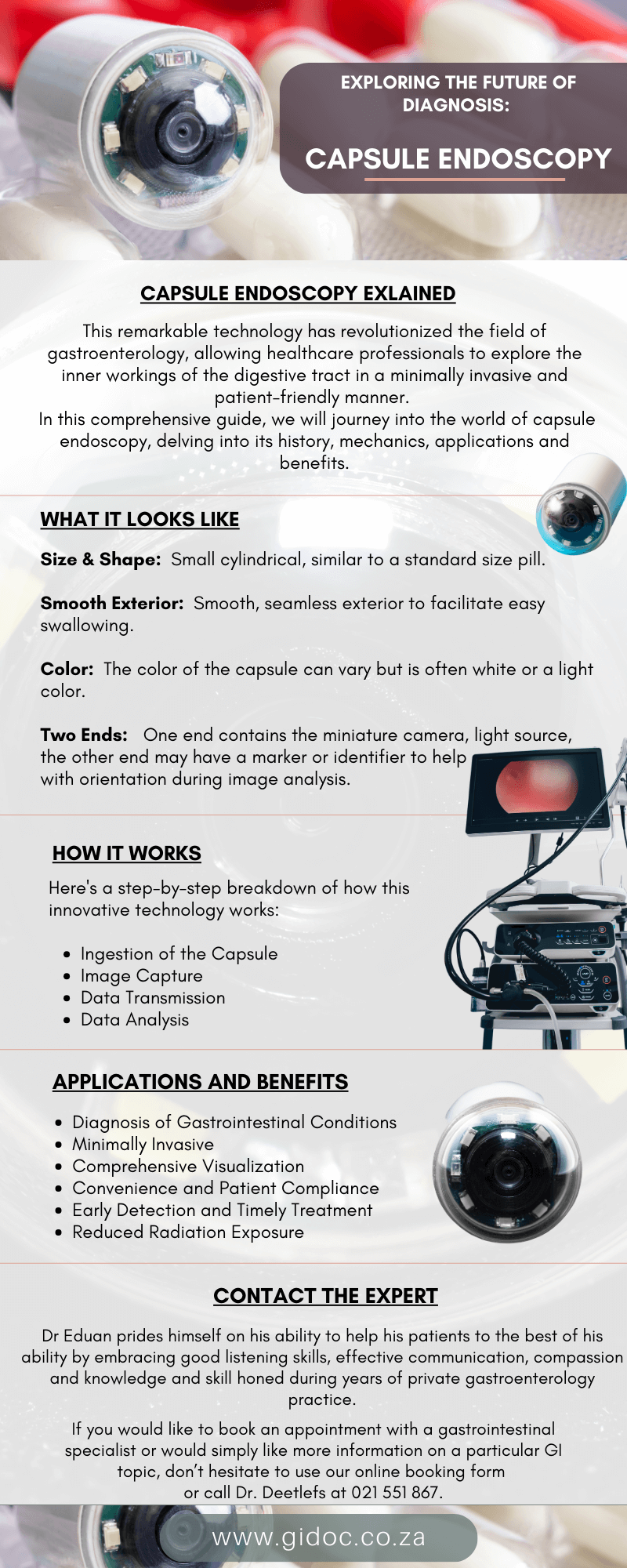
- Capsule endoscopy or ultrasound when needed
Treatment Options
Managing IBS
IBS is usually managed with a multi-faceted approach aimed at reducing symptom frequency and improving quality of life:
- Low-FODMAP diet to reduce gas-producing foods
- Fiber supplements for constipation-predominant IBS (soluble fiber preferred)
- Antispasmodic medications like hyoscine or dicyclomine
- Laxatives or anti-diarrheal agents as needed
- Probiotics to balance gut bacteria
- Cognitive behavioral therapy (CBT) or gut-directed hypnotherapy
- Stress management with mindfulness, yoga, or regular exercise
Managing IBD
IBD requires targeted medical therapy to control inflammation and induce remission:
- Aminosalicylates (5-ASA) for mild to moderate UC
- Corticosteroids for moderate to severe flares
- Immunomodulators like azathioprine or methotrexate for long-term control
- Biologic therapies (anti-TNF agents, integrin inhibitors, IL-12/23 blockers)
- Janus kinase (JAK) inhibitors for refractory cases
- Nutritional therapy or enteral nutrition in pediatric cases
- Surgical options including colectomy or bowel resection when necessary
Living with IBS or IBD
Coping with IBS
While IBS does not cause damage to the digestive tract, the chronic and unpredictable nature of symptoms can lead to anxiety, embarrassment, and a lower quality of life.
Supportive care, patient education, and tailored diet and lifestyle changes can significantly improve symptoms.
Coping with IBD
IBD is a lifelong condition that can fluctuate between remission and flare-ups. Early diagnosis, consistent treatment, and lifestyle adjustments can help prevent complications and maintain gut health.
Patients benefit from ongoing support from a gastroenterology care team.
General Tips for Both
- Track symptoms and dietary triggers with a health diary
- Build a strong relationship with your healthcare provider
- Avoid smoking and unnecessary NSAIDs
- Prioritize mental health care and support networks
When to See a Gastroenterologist
You should see a gastroenterologist if you experience:
- Persistent abdominal pain or bloating
- Blood or mucus in the stool
- Unexplained weight loss
- Severe or frequent diarrhea
- Fatigue or anemia
- Any symptoms interfering with your day-to-day life
Early consultation can lead to faster diagnosis and improved outcomes, especially in cases of IBD.
Conclusion: IBS and IBD Are Not the Same
Although IBS and IBD can produce overlapping symptoms, they differ significantly in cause, severity, and long-term risks.
IBS is a functional disorder, often manageable through lifestyle changes and stress reduction. IBD, on the other hand, is a chronic inflammatory disease that can result in serious complications without medical intervention.
Understanding these differences empowers patients to seek timely care and take control of their digestive health.
If you’re unsure whether your symptoms point to IBS or IBD, schedule a consultation with a gastroenterologist. An accurate diagnosis is the first step toward effective treatment and lasting relief.
Contact the Experts
Dr. Deetlefs has earned the reputation of a trusted health expert providing consultative, diagnostic, and therapeutic endoscopic and related services to patients in Cape Town and beyond.
Dr. Deetlefs can be contacted to confirm the estimated breakdown should you be interested in having the procedure done.
DISCLAIMER: PLEASE READ CAREFULLY
The information on this website is to provide general guidance. In no way does any of the information provided reflect definitive medical advice and self-diagnoses should not be made based on information obtained online. It is important to consult a Gastroenterologist or medical doctor regarding ANY and ALL symptoms or signs including, but not limited to: abdominal pain, haemorrhoids or anal / rectal bleeding as it may a sign of a serious illness or condition. A thorough consultation and examination should ALWAYS be performed for an accurate diagnosis and treatment plan. Be sure to call a physician or call our office today and schedule a consultation.
© Dr. Eduan Deetlefs, Registered Gastroenterologist, GI Doc Cape Town
Our website information is not intended or implied to be a substitute for professional medical advice, diagnosis or treatment. Please consult a doctor about your specific condition. Only a trained physician can determine an accurate diagnosis and proper treatment.