Understanding a Polypectomy: Risks, Benefits, and Recovery
What Is a Polypectomy?
A polypectomy is a medical procedure in which a polyp, or small growth, is removed from the body.
Polyps can occur in a variety of places, including the colon, nose, and throat.
A Polypectomy is procedure used by doctors to remove polyps from the inner linings of the large intestine/the colon. It is usually performed during colonoscopy or sigmoidoscopy.
A colonoscopy is first done to detect the presence of any polyps. If any are detected, a polypectomy is performed, and the tissue is removed.
The tissue will be examined to determine if the growths are cancerous, precancerous, or benign to prevent colon cancer.
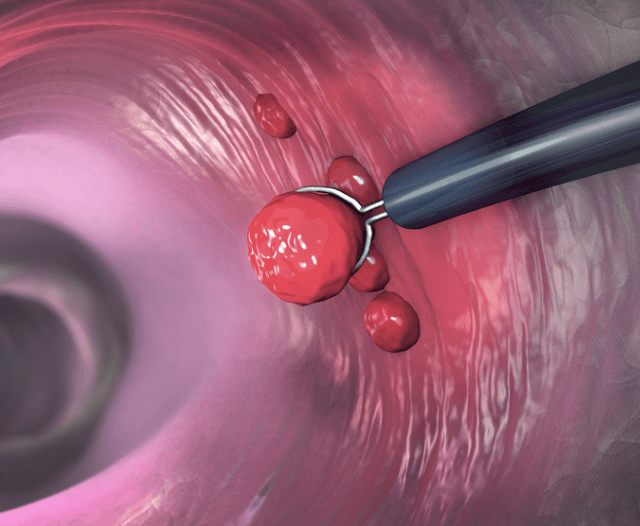
Polyps can be small, large, sessile, or pedunculated. Sessile polyps are flat and don’t have a stalk. Pedunculated polyps grow on stalks like mushrooms.
For small polyps (less than 5mm in diameter), biopsy forceps can be used for removal. Larger polyps (up to 2cm in diameter) can be removed using a snare.
After the procedure, your Gastroenterologist will remove the colonoscope and give you a chance to change and rest.
The medical staff will give you instructions explaining what to expect and the symptoms to look out for.
In most cases, polyps are benign, or non-cancerous. However, some polyps may be precancerous, or have the potential to develop into cancer.
Polypectomies are typically performed as outpatient procedures, meaning the patient does not need to stay overnight in the hospital.
The specific procedure will vary depending on the location of the polyp.
For example, a polyp in the colon may be removed during a colonoscopy, while a polyp in the nose may be removed with a nasal endoscope.
In this blog article we discuss the polypectomy procedure, risks and benefits involved.
What is a Polyp?
A polyp is a small, benign growth that protrudes from the surface of a mucous membrane.
Polyps can occur anywhere in the body where there is mucous membrane, but they are most commonly found in the nose, sinuses, and colon.
While most polyps are benign, some can become cancerous. Polyps are usually treated by removal, either by surgery or endoscopy.
Types of Polypectomies
There are several different types of polypectomies, depending on the location and type of polyp being removed.
The most common type of polypectomy is a colonoscopy, in which polyps are removed from the colon (large intestine).
Other types of polypectomies include endometrial polypectomies (removal of polyps from the lining of the uterus), gastric polypectomies (removal of polyps from the stomach), and bronchial polypectomies (removal of polyps from the airway).
What Are the Risks of a Polypectomy?
A polypectomy is a minimally invasive surgical procedure used to remove polyps from the colon.
Polyps are growths that can develop on the lining of the colon.
While most polyps are benign, or noncancerous, some can develop into cancer.
The risks of a polypectomy include:
- Bleeding
- Infection
- Perforation of the colon
Bleeding is the most common complication, and usually occurs during or immediately after the procedure.
Infection and perforation are rare but more serious complications that can occur. Infection can develop if the colon is not properly cleaned before the procedure.
Perforation can occur if the polyp is removed without proper cautery, or if the colon is nicked during the procedure.
Overall, the risks of a polypectomy are low. The procedure is typically safe, and complications are rare.
However, as with any surgical procedure, there are potential risks that should be discussed with your doctor prior to having the procedure.
What Are the Benefits of Undergoing a Polypectomy?
Polyps can be benign (noncancerous) or malignant (cancerous), and although most polyps are benign, removal is still recommended because some polyps can develop into cancer over time.
There are several benefits of undergoing a polypectomy.
First, it can help to prevent colon cancer by removing precancerous polyps before they have a chance to become cancerous.
Second, it can help to relieve symptoms such as bleeding or changes in bowel habits that may be caused by polyps.
Third, it can help to improve the overall health of the colon by removing polyps that could potentially cause problems in the future.
Overall, a polypectomy is a safe and effective way to remove polyps from the colon or rectum.
If you have any concerns about polyps or your risk for colon cancer, be sure to talk to your doctor.
What Is Recovery Like After a Polypectomy?
Recovery from a polypectomy is typically fairly easy, and most people can go home the same day as the procedure. However, there are a few things you can do to help make the recovery process go more smoothly.
Recovery is generally quick. Minor side effects such as gassiness, bloating, and cramps usually resolve within 24 hours.
With a more involved procedure, a full recovery can take up to two weeks.
First, it’s important to get plenty of rest. This will help your body heal and reduce the risk of complications.
You should also take it easy for the first few days after the procedure. Avoid strenuous activity and heavy lifting. Drink plenty of fluids and eat a healthy diet to help your body recover.
If you have any pain, your doctor may prescribe medication. Be sure to take it as directed. You may also have some bleeding or drainage from the incision site.
This is normal and should eventually stop. If you have any concerns about your recovery, be sure to contact your doctor.

Signs You Might Need a Polypectomy
If you have been diagnosed with a polyp, your doctor may recommend a polypectomy to remove it.
However, not all polyps need to be removed and your doctor will determine if a polypectomy is necessary.
There are a few signs that may indicate that you need a polypectomy, which include:
- If the polyp is large
- If the polyp is bleeding
- If the polyp is causing pain or other symptoms
- If the polyp is located in a difficult to reach area
If you have any of these signs, your doctor will likely recommend a polypectomy.
During the procedure, a small camera is inserted into the colon and the polyp is removed.
A polypectomy is generally a safe and effective procedure with a low risk of complications.

How You Can Prevent Polyps
There are a few things you can do to help prevent polyps from forming in the first place.
First, eat a healthy diet that is low in fat and sugar. Get plenty of fiber from whole grains, fruits, and vegetables.
Second, exercise regularly.
Third, avoid smoking.
And fourth, if you drink alcohol, do so in moderation.
If you have any family members with polyps or other gastrointestinal problems, be sure to let your doctor know.

Conclusion
The most important thing to do after a polypectomy is to maintain a healthy lifestyle.
This means eating a healthy diet, getting enough sleep, and exercising. Doing these things will help to lower the risk of polyps from returning.
If you have any questions or concerns regarding a polypectomy, please contact your physician.
For any additional information regarding a polypectomy, it’s best to find a trusted and experienced Gastroenterologist who can answer your questions clearly, recommend appropriate solutions, and perform tests with precision and expertise.
Dr. Deetlefs has earned the reputation of a trusted health expert providing consultative, diagnostic, and therapeutic endoscopic and related services to patients in Cape Town and beyond.
Dr. Deetlefs can be contacted to confirm the estimated breakdown should you be interested in having the procedure done.
DISCLAIMER: PLEASE READ CAREFULLY
The information on this website is to provide general guidance. In no way does any of the information provided reflect definitive medical advice and self-diagnoses should not be made based on information obtained online. It is important to consult a Gastroenterologist or medical doctor regarding ANY and ALL symptoms or signs including, but not limited to: abdominal pain, haemorrhoids or anal / rectal bleeding as it may a sign of a serious illness or condition. A thorough consultation and examination should ALWAYS be performed for an accurate diagnosis and treatment plan. Be sure to call a physician or call our office today and schedule a consultation.
© Dr. Eduan Deetlefs, Registered Gastroenterologist, GI Doc Cape Town
Our website information is not intended or implied to be a substitute for professional medical advice, diagnosis or treatment. Please consult a doctor about your specific condition. Only a trained physician can determine an accurate diagnosis and proper treatment.