Stress and the Gut: Understanding the Brain-Gut Connection
When we think of stress, we often associate it with racing thoughts, increased heart rate, or anxiety. But did you know that stress has a profound impact on your digestive system too? If you’ve ever felt “butterflies” in your stomach before a big presentation or experienced nausea during a stressful situation, you’ve already encountered the brain-gut connection.
In recent years, the relationship between mental health and gastrointestinal (GI) health has become a major focus in medical research and clinical practice. Scientists now understand that the gut and brain are in constant communication—a relationship often referred to as the brain-gut axis. Understanding this connection is vital for patients with chronic digestive issues, as well as for healthcare professionals managing gastrointestinal conditions.
In this article, we’ll explore the fascinating link between stress and the gut, discuss how stress impacts various digestive conditions, and offer strategies for supporting both mental and digestive health.
What Is the Brain-Gut Axis?
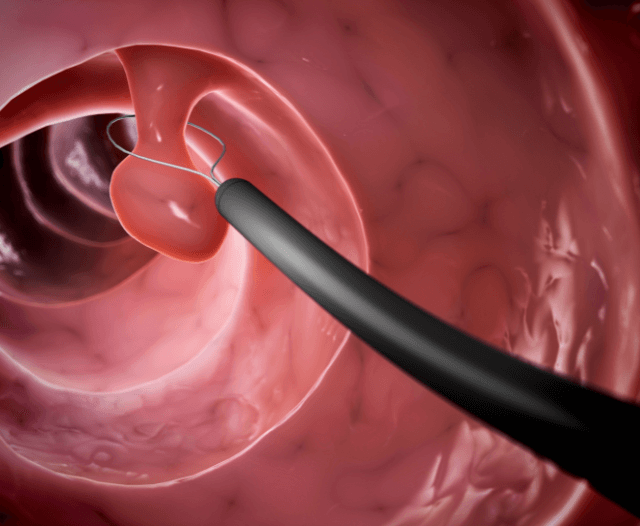
The brain-gut axis is a complex, bidirectional communication system between the central nervous system (CNS) and the enteric nervous system (ENS), which is sometimes called the “second brain” of the body.
The ENS is a vast network of neurons embedded in the walls of the gastrointestinal tract. It controls digestive processes such as peristalsis (the movement of food through the gut), enzyme secretion, blood flow, and nutrient absorption—often independent of conscious thought. The brain and gut communicate through a series of biochemical signals, including:
- Neurotransmitters: Like serotonin and dopamine, which influence both mood and gut function.
- Hormones: Such as cortisol, the body’s primary stress hormone.
- Immune system responses: Inflammation can be triggered or suppressed by signals from the gut or brain.
- Vagus nerve: The longest cranial nerve, it serves as a direct highway between the brain and the digestive tract.
This communication loop ensures that emotional and psychological states can influence digestive health—and vice versa.
How Stress Affects the Digestive System
Stress is the body’s natural response to perceived threats. In small amounts, it can be beneficial. However, chronic stress—like that caused by work pressure, unresolved trauma, or mental health conditions—can wreak havoc on the digestive system. Here are some keyways stress affects gut function:
1. Changes in Motility
Stress can either speed up or slow down the movement of food through the digestive tract. This can lead to symptoms like diarrhea, constipation, bloating, and cramping. In irritable bowel syndrome (IBS), stress is a major trigger for flare-ups.
2. Increased Gut Permeability
Often referred to as “leaky gut,” stress may increase the permeability of the intestinal wall, allowing toxins, bacteria, and undigested food particles to enter the bloodstream. This can trigger inflammation and immune responses that worsen GI symptoms.
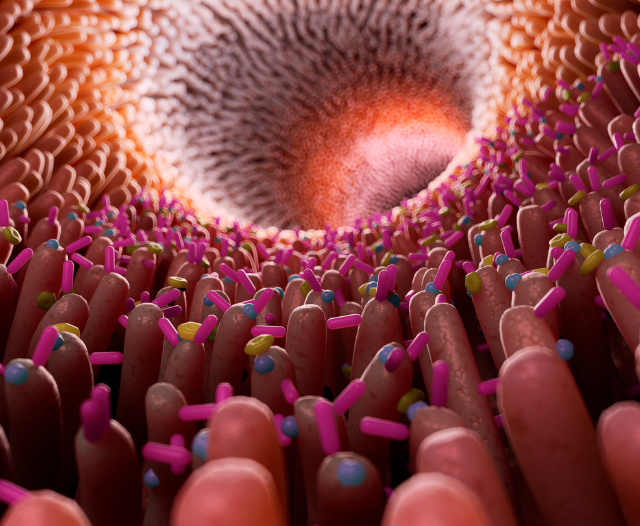
3. Altered Gut Microbiome
The trillions of bacteria residing in the gut (the microbiota) are essential for digestive and immune function. Chronic stress can alter the composition of these microbes, reducing beneficial strains and allowing harmful bacteria to thrive—an imbalance known as dysbiosis.
4. Enhanced Perception of Pain
Stress may increase sensitivity to pain in the gastrointestinal tract, a phenomenon known as visceral hypersensitivity. This makes mild symptoms feel more severe, a common experience in functional GI disorders like IBS.
5. Increased Acid Production
Acute stress can raise stomach acid levels, increasing the risk of acid reflux, gastritis, or peptic ulcers. Over time, this may contribute to chronic GI conditions.

The Role of Stress in GI Conditions
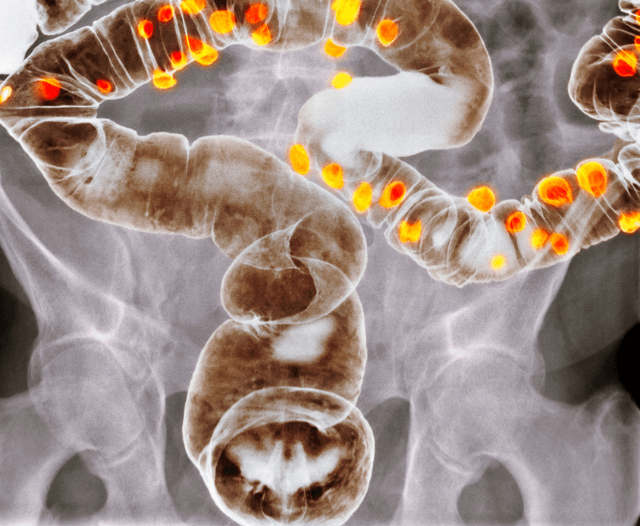
Many chronic digestive disorders have a psychosomatic component—meaning they are influenced by psychological stress. Below are some GI conditions that are commonly affected:
Irritable Bowel Syndrome (IBS)
IBS is one of the most common functional GI disorders, affecting 10–15% of people worldwide. While the exact cause remains unknown, stress is recognized as a major factor that influences both the onset and severity of IBS symptoms, including:
- Abdominal pain
- Gas and bloating
- Constipation or diarrhea
- Changes in bowel habits
Inflammatory Bowel Disease (IBD)
While IBD (which includes Crohn’s disease and ulcerative colitis) is primarily an autoimmune condition, stress can exacerbate symptoms and potentially influence disease progression. Research suggests that high stress levels can trigger flare-ups or interfere with the body’s ability to heal during remission.
Functional Dyspepsia
This condition causes upper abdominal discomfort, often without any identifiable structural abnormality. Stress and anxiety are major contributors to symptoms like early satiety, bloating, and nausea.
GERD (Gastroesophageal Reflux Disease)
Stress can relax the lower esophageal sphincter and increase stomach acid, leading to more frequent reflux symptoms.
The Impact of Mental Health Disorders on Gut Health
Depression and anxiety are commonly associated with chronic digestive issues. People suffering from these mental health conditions often report more severe GI symptoms, even when medical tests show no clear abnormalities.
This relationship is a two-way street. Just as stress and anxiety can worsen gut symptoms, persistent GI issues can negatively affect mental health, contributing to a cycle of discomfort and emotional distress.

The Microbiome and Mood: The Emerging Role of Psychobiotics
The gut microbiome plays a key role in regulating mood and emotional well-being. Certain gut bacteria produce neurotransmitters like serotonin and gamma-aminobutyric acid (GABA), which influence mood and stress response.
This has led to the development of psychobiotics—probiotics and prebiotics that positively impact mental health. While research is still ongoing, early studies suggest that supplementing with specific probiotic strains may reduce anxiety, improve mood, and enhance cognitive function.
Managing Stress for Better Digestive Health
If you struggle with chronic digestive issues, addressing stress is a crucial part of your treatment plan. Here are evidence-based strategies to help manage stress and support gut health:
1. Mindfulness and Meditation
Mindfulness-based practices like meditation, deep breathing, and body scanning have been shown to reduce cortisol levels and calm the nervous system. Regular practice may reduce symptom severity in conditions like IBS.
2. Cognitive Behavioral Therapy (CBT)
CBT is a type of talk therapy that helps individuals change negative thought patterns and behaviors. Studies show that CBT can significantly improve symptoms in IBS and other functional GI disorders.
3. Exercise
Regular physical activity boosts endorphins, reduces inflammation, and supports digestion. Low-impact exercises like walking, yoga, or swimming are particularly beneficial.
4. Gut-Healthy Diet
Eating a balanced diet rich in fiber, fermented foods (like yogurt and kefir), and anti-inflammatory nutrients can support a healthy microbiome and improve resilience to stress.
5. Adequate Sleep
Sleep disturbances increase stress and worsen GI symptoms. Prioritize 7–9 hours of restful sleep each night and maintain a regular sleep schedule.
When to Seek Medical Help
While stress management is essential, persistent or severe digestive symptoms should never be ignored. You should see a gastroenterologist if you experience:
- Unexplained weight loss
- Blood in the stool
- Severe or persistent abdominal pain
- Difficulty swallowing
- Changes in bowel habits lasting more than a few weeks
A specialist can help determine whether your symptoms are functional or due to an underlying condition that requires medical treatment.

Conclusion
The connection between stress and the gut is more than a passing feeling—it’s a complex, dynamic relationship that plays a vital role in your overall health. Whether you’re dealing with a chronic GI condition or simply want to optimize your digestive well-being, understanding the brain-gut axis is a powerful step in the right direction.
By addressing both emotional and digestive health together, patients can take a more holistic approach to healing, symptom management, and long-term wellness.
If stress is impacting your gut health, speak to a gastroenterologist or integrative care provider about comprehensive solutions that support both body and mind.
Get in Touch
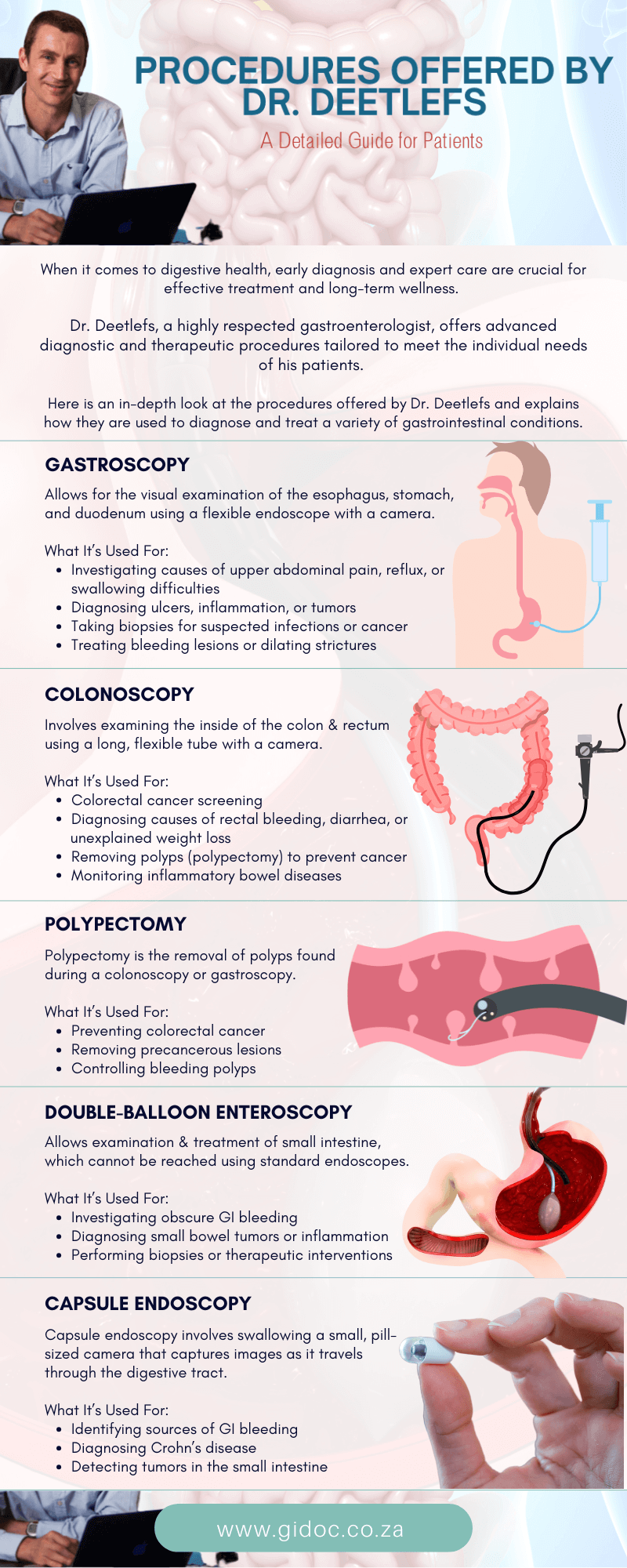
Dr. Deetlefs has earned the reputation of a trusted health expert providing consultative, diagnostic, and therapeutic endoscopic and related services to patients in Cape Town and beyond.
Dr. Deetlefs can be contacted to confirm the estimated breakdown should you be interested in having the procedure done.
DISCLAIMER: PLEASE READ CAREFULLY
The information on this website is to provide general guidance. In no way does any of the information provided reflect definitive medical advice and self-diagnoses should not be made based on information obtained online. It is important to consult a Gastroenterologist or medical doctor regarding ANY and ALL symptoms or signs including, but not limited to: abdominal pain, haemorrhoids or anal / rectal bleeding as it may a sign of a serious illness or condition. A thorough consultation and examination should ALWAYS be performed for an accurate diagnosis and treatment plan. Be sure to call a physician or call our office today and schedule a consultation.
© Dr. Eduan Deetlefs, Registered Gastroenterologist, GI Doc Cape Town
Our website information is not intended or implied to be a substitute for professional medical advice, diagnosis or treatment. Please consult a doctor about your specific condition. Only a trained physician can determine an accurate diagnosis and proper treatment.