What to Expect During a Gastroscopy Procedure: Step-by-Step Guide
Introduction
For individuals facing gastrointestinal issues, the prospect of undergoing a gastroscopy procedure can be both daunting and mysterious.
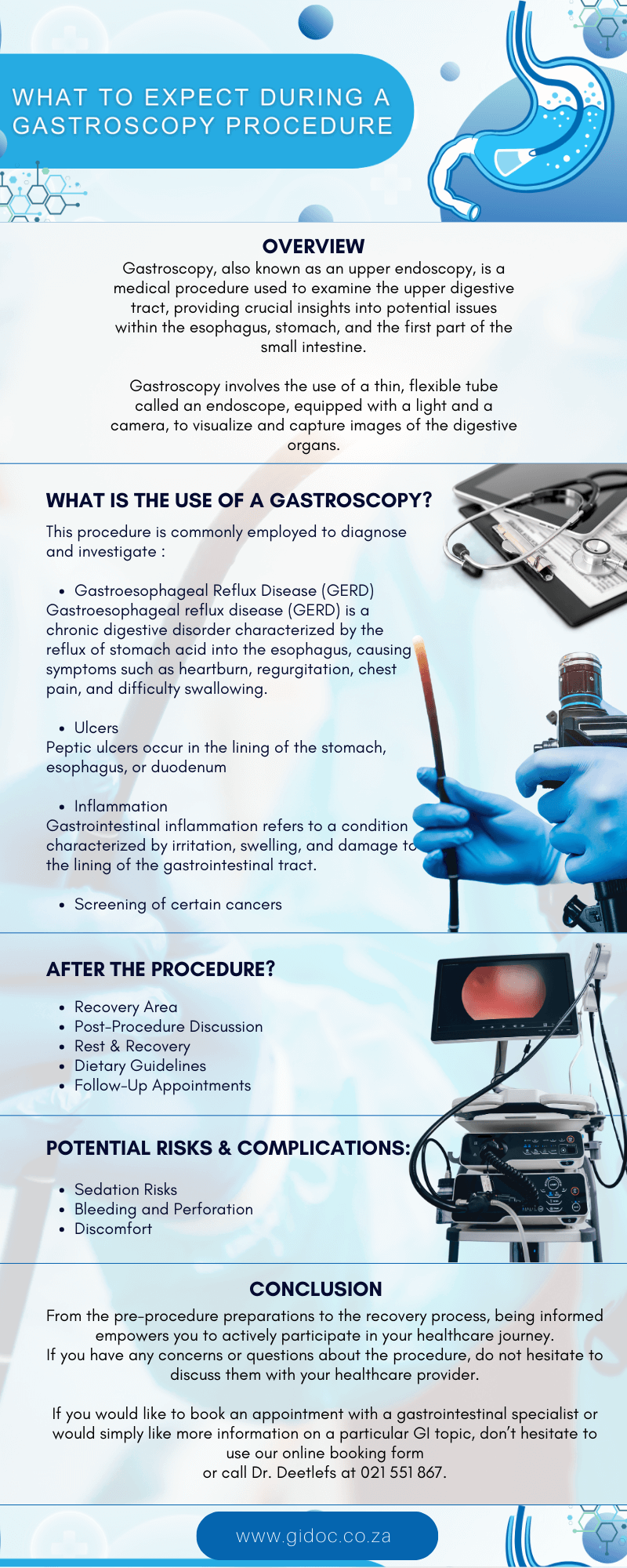
Gastroscopy, also known as an upper endoscopy, is a medical procedure used to examine the upper digestive tract, providing crucial insights into potential issues within the esophagus, stomach, and the first part of the small intestine.
In this comprehensive guide, we will walk you through what to expect during a gastroscopy procedure, step by step, alleviating uncertainties and empowering you with knowledge.
What is Gastroscopy?
Gastroscopy involves the use of a thin, flexible tube called an endoscope, equipped with a light and a camera, to visualize and capture images of the digestive organs.
This procedure is commonly employed to diagnose and investigate various gastrointestinal conditions, including gastroesophageal reflux disease (GERD), ulcers, inflammation, and even to screen for certain cancers.
Gastroesophageal reflux disease:
Gastroesophageal reflux disease (GERD) is a chronic digestive disorder characterized by the reflux of stomach acid into the esophagus, causing symptoms such as heartburn, regurgitation, chest pain, and difficulty swallowing.
It occurs when the lower esophageal sphincter (LES)—a muscular ring at the junction between the esophagus and the stomach—does not function properly, allowing stomach contents to flow back up into the esophagus.
Ulcer: An ulcer is a type of open sore or lesion that forms on the skin or mucous membranes of the body.
When discussing ulcers in the context of gastrointestinal health, we typically refer to peptic ulcers, which occur in the lining of the stomach, esophagus, or duodenum (the first part of the small intestine).
Gastrointestinal inflammation:
Gastrointestinal inflammation refers to a condition characterized by irritation, swelling, and damage to the lining of the gastrointestinal tract.
This inflammation can affect various parts of the digestive system, including the esophagus, stomach, small intestine, and large intestine.
It can be caused by a wide range of factors, including infections, autoimmune disorders, dietary factors, and medications.
Before the Procedure
Preparation Instructions:
Before the gastroscopy, your healthcare provider will provide detailed instructions on how to prepare for the procedure.
This may include fasting for a specific period, typically overnight, to ensure a clear view of the digestive tract.
Medication Adjustments:
Inform your healthcare provider about any medications you are currently taking, especially blood thinners or anticoagulants.
In some cases, adjustments to your medication regimen may be necessary before the procedure.
Health Assessment:
A pre-procedure health assessment will be conducted to ensure that you are physically prepared for the gastroscopy.
This may involve checking vital signs, reviewing your medical history, and addressing any concerns you may have.
The Gastroscopy Procedure
Arrival at the Medical Facility:
On the day of the procedure, you will check in at the medical facility. The healthcare team will guide you through the necessary paperwork and answer any last-minute questions you may have.
Consent and Explanation:
Before the procedure, you will meet with the gastroenterologist or endoscopist who will perform the gastroscopy.
They will explain the procedure in detail, discuss its purpose, and address any concerns you might have. You will be asked to sign a consent form indicating your understanding and agreement to undergo the procedure.
Administration of Anesthesia:
Gastroscopy is typically performed under sedation to ensure your comfort and relaxation during the procedure. You may receive an intravenous (IV) sedative, and in some cases, a local anesthetic to numb the throat.
Positioning:
Once sedated, you will be positioned on your left side. A mouthguard may be placed to protect your teeth and the endoscope.
Insertion of the Endoscope:
The endoscope, a thin, flexible tube with a light and camera at its tip, will be gently inserted through your mouth and guided down the esophagus.
The camera transmits real-time images to a monitor, allowing the healthcare team to examine the lining of the digestive organs.
Visual Examination:
The gastroenterologist will carefully navigate the endoscope through the esophagus, stomach, and the initial part of the small intestine.
They will inspect the mucosal lining for abnormalities such as inflammation, ulcers, tumors, or other structural issues.
Biopsy (if necessary):
During the procedure, the gastroenterologist may take tissue samples (biopsies) for further examination.
This is a routine and relatively painless process. Biopsies can provide valuable information about the presence of infections, inflammation, or abnormalities.
Air Insufflation:
To enhance visibility, air may be gently introduced through the endoscope into the digestive tract. This can cause a temporary feeling of fullness or bloating.
Completion of Procedure:
Once the examination is complete, the endoscope will be carefully removed. You will be monitored as you recover from the sedation.
After the Procedure
Recovery Area:
You will be taken to a recovery area where you will be monitored as the sedation wears off. It is common to experience a mild sore throat or bloating due to the air insufflation.
Post-Procedure Discussion:
The gastroenterologist will meet with you to discuss their initial findings and share any immediate insights. If biopsies were taken, the results may take a few days and will be communicated to you in a follow-up appointment.
Rest and Recovery:
It’s advisable to rest for the remainder of the day. You should refrain from driving or making important decisions until the effects of the sedation wear off completely.
Dietary Guidelines:
You may be advised to start with a light diet and gradually resume your regular eating habits. Avoiding hot or spicy foods, as well as heavy or greasy meals, can help ease any residual discomfort.
Follow-Up Appointments:
Your healthcare provider will schedule a follow-up appointment to discuss the complete results of the gastroscopy, including any biopsy findings, and to determine the next steps in your care.
Potential Risks and Complications
While gastroscopy is generally considered safe, it is important to be aware of potential risks and complications associated with the procedure:
- Sedation Risks: The use of sedative medications during gastroscopy carries a risk of complications, such as respiratory depression, cardiovascular events, or allergic reactions. However, these risks are minimal and are carefully monitored by the healthcare team.
- Bleeding and Perforation: In rare cases, gastroscopy may cause bleeding or perforation of the gastrointestinal tract, particularly if therapeutic interventions are performed. However, the risk of these complications is low, especially when the procedure is performed by experienced gastroenterologists.
- Discomfort: Some patients may experience mild discomfort or a gagging sensation during the insertion of the endoscope. However, sedation is typically administered to minimize discomfort and ensure patient comfort throughout the procedure.
After the Procedure
After the gastroscopy, you will be taken to a recovery area where you will be monitored as the effects of the sedation wear off.
You may experience some temporary side effects, such as a sore throat, bloating, or mild discomfort.
The healthcare team will provide instructions for post-procedure care, including dietary guidelines, activity restrictions, and when to follow up with your healthcare provider.
Conclusion
Navigating the unknowns of a gastroscopy procedure becomes more manageable with a comprehensive understanding of each step.
From the pre-procedure preparations to the recovery process, being informed empowers you to actively participate in your healthcare journey.
If you have any concerns or questions about the procedure, do not hesitate to discuss them with your healthcare provider.
Remember, the goal of a gastroscopy is to provide valuable insights into your digestive health, helping guide further diagnosis and treatment decisions.
Contact Dr. Deetlefs
Dr. Deetlefs has earned the reputation of a trusted health expert providing consultative, diagnostic, and therapeutic endoscopic and related services to patients in Cape Town and beyond.
Dr. Deetlefs can be contacted to confirm the estimated breakdown should you be interested in having the procedure done.
DISCLAIMER: PLEASE READ CAREFULLY
The information on this website is to provide general guidance. In no way does any of the information provided reflect definitive medical advice and self-diagnoses should not be made based on information obtained online. It is important to consult a Gastroenterologist or medical doctor regarding ANY and ALL symptoms or signs including, but not limited to: abdominal pain, haemorrhoids or anal / rectal bleeding as it may a sign of a serious illness or condition. A thorough consultation and examination should ALWAYS be performed for an accurate diagnosis and treatment plan. Be sure to call a physician or call our office today and schedule a consultation.
© Dr. Eduan Deetlefs, Registered Gastroenterologist, GI Doc Cape Town
Our website information is not intended or implied to be a substitute for professional medical advice, diagnosis or treatment. Please consult a doctor about your specific condition. Only a trained physician can determine an accurate diagnosis and proper treatment.