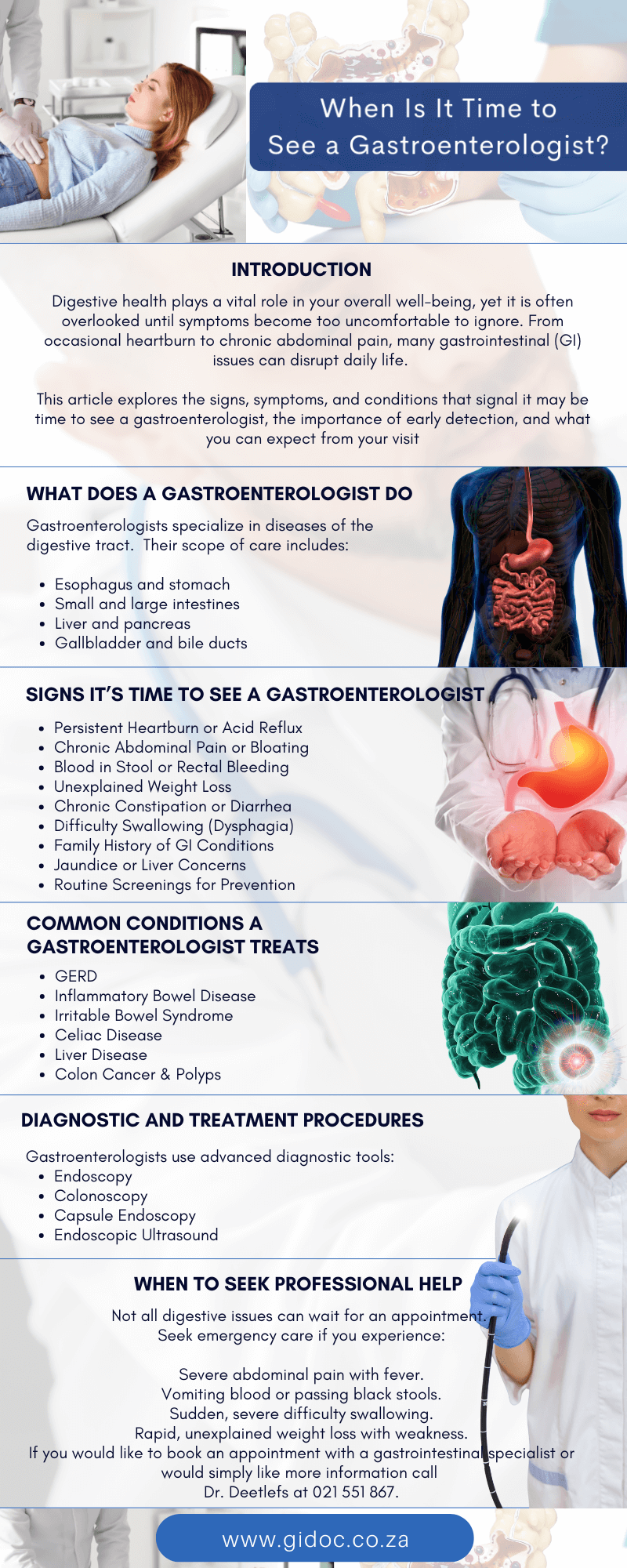
When Is It Time to See a Gastroenterologist?
Introduction
Digestive health plays a vital role in your overall well-being, yet it is often overlooked until symptoms become too uncomfortable to ignore. From occasional heartburn to chronic abdominal pain, many gastrointestinal (GI) issues can disrupt daily life.
But how do you know when it’s time to move beyond over-the-counter remedies and consult a specialist?
A gastroenterologist is a physician trained in diagnosing and treating disorders of the digestive system, which includes the esophagus, stomach, intestines, liver, pancreas, and gallbladder. Knowing when to seek expert care can make all the difference between managing symptoms effectively and allowing conditions to worsen.
This article explores the signs, symptoms, and conditions that signal it may be time to see a gastroenterologist, the importance of early detection, and what you can expect from your visit.
What Does a Gastroenterologist Do?
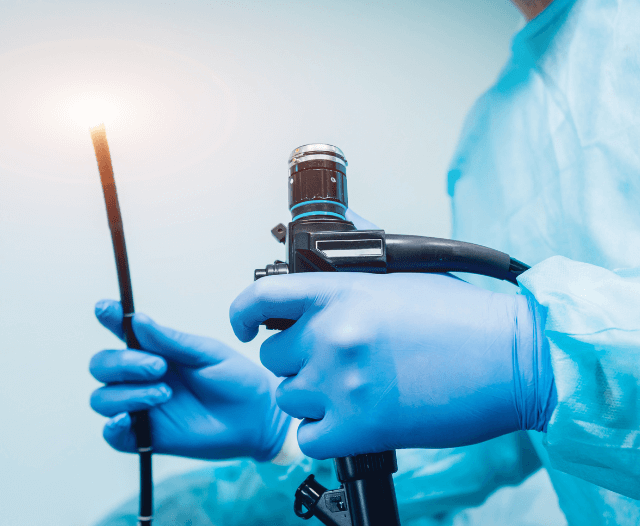
Gastroenterologists specialize in diseases of the digestive tract and perform advanced procedures such as endoscopy and colonoscopy.
Their scope of care includes:
- Esophagus and stomach: GERD, ulcers, swallowing disorders.
- Small and large intestines: Crohn’s disease, ulcerative colitis, irritable bowel syndrome (IBS), strictures.
- Liver and pancreas: Hepatitis, fatty liver disease, pancreatitis.
- Gallbladder and bile ducts: Gallstones, bile duct obstructions.
- Cancer prevention and detection: Screening for colorectal cancer and Barrett’s esophagus.
If you experience ongoing or severe digestive issues, a gastroenterologist provides specialized care that general practitioners may not offer.

Signs It’s Time to See a Gastroenterologist
1. Persistent Heartburn or Acid Reflux
Occasional heartburn after a spicy meal is common, but frequent reflux may signal gastroesophageal reflux disease (GERD). Left untreated, GERD can damage the esophagus and increase the risk of Barrett’s esophagus and esophageal cancer. If heartburn occurs more than twice a week, it’s time to see a gastroenterologist.
2. Chronic Abdominal Pain or Bloating
Stomach discomfort should not be ignored if it:
- Lasts more than a few days,
- Is associated with changes in bowel habits, or
- Comes with nausea, vomiting, or weight loss.
These symptoms may indicate IBS, IBD (Crohn’s or ulcerative colitis), ulcers, or gallstones.
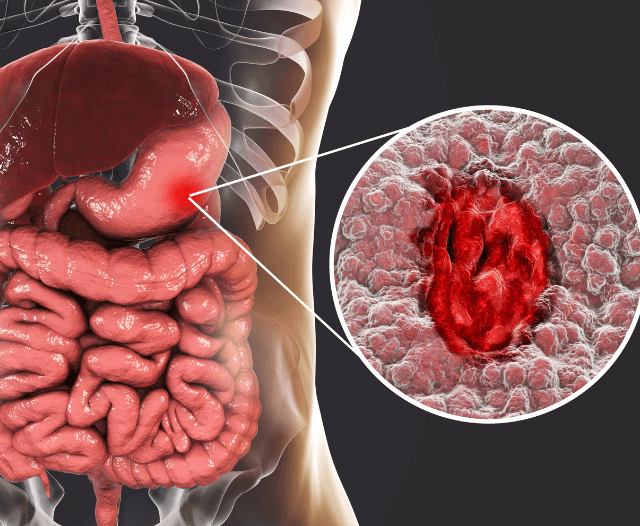
3. Blood in Stool or Rectal Bleeding
Visible blood in your stool—or stools that are black and tarry—requires immediate medical evaluation. Causes may range from hemorrhoids to more serious conditions such as colon polyps, colorectal cancer, or inflammatory bowel disease.
4. Unexplained Weight Loss
Losing weight without changing your diet or exercise routine can be a red flag. A gastroenterologist can investigate causes such as celiac disease, Crohn’s disease, pancreatic disorders, or even gastrointestinal cancers.
5. Chronic Constipation or Diarrhea
Persistent changes in bowel habits should not be dismissed. Constipation lasting weeks, or diarrhea that doesn’t resolve, may point to IBS, infections, strictures, or even colon cancer.
6. Difficulty Swallowing (Dysphagia)
If swallowing feels painful or food seems to get “stuck,” it could be related to esophageal strictures, GERD complications, or motility disorders. Early diagnosis helps prevent complications such as malnutrition or aspiration.
7. Family History of GI Conditions
If colorectal cancer, polyps, Crohn’s disease, or celiac disease runs in your family, your risk is higher. Regular check-ups with a gastroenterologist can provide personalized screening and prevention strategies.
8. Jaundice or Liver Concerns
Yellowing of the skin or eyes is a warning sign of liver disease. Other symptoms include dark urine, light-colored stools, or persistent fatigue. Conditions like hepatitis, cirrhosis, and fatty liver disease require specialist management.
9. Routine Screenings for Prevention
Even without symptoms, adults should see a gastroenterologist for preventive care:
- Colonoscopy at age 45+ (earlier if family history exists).
- Periodic follow-up if polyps are found.
- Endoscopy for patients with long-standing GERD.
Routine screenings save lives by detecting cancer and precancerous conditions early.
Common Conditions a Gastroenterologist Treats
Gastroesophageal Reflux Disease (GERD)
Symptoms: Heartburn, regurgitation, chronic cough.
Why see a GI specialist? To prevent esophageal damage and complications.
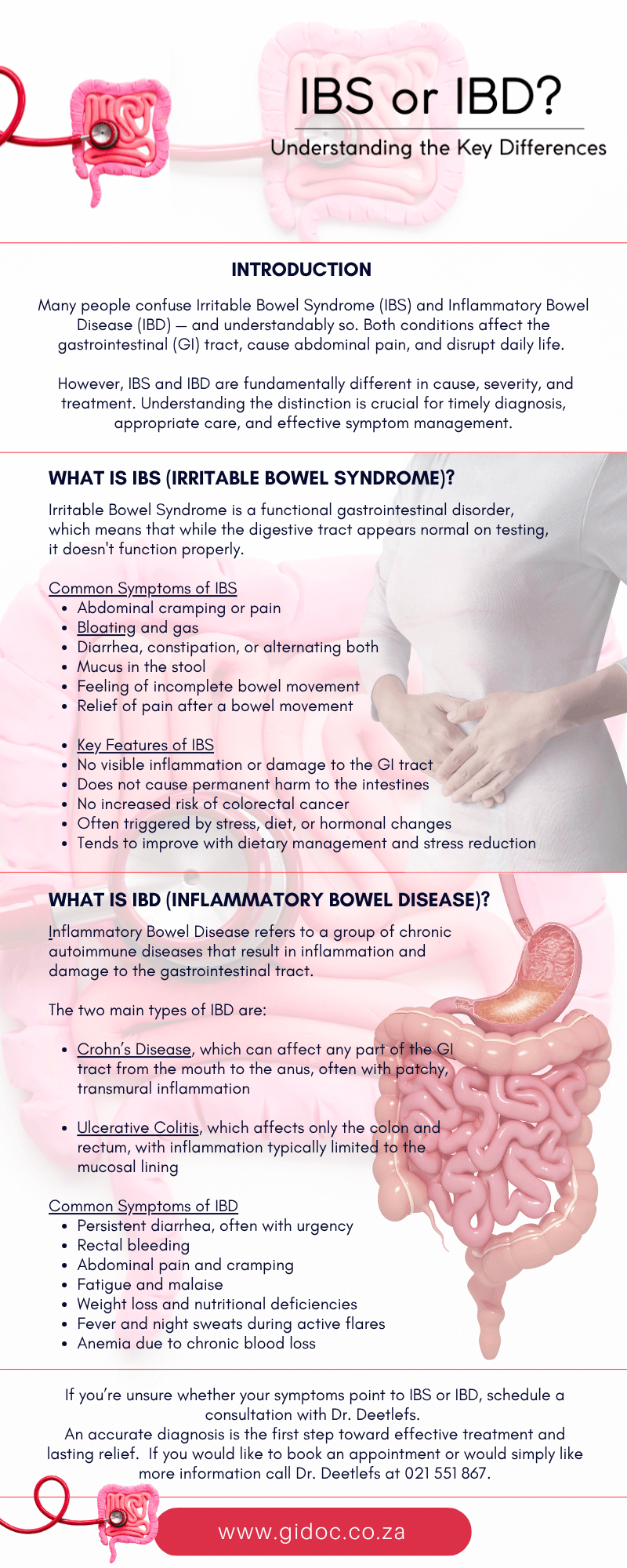
Inflammatory Bowel Disease (Crohn’s Disease & Ulcerative Colitis)
Symptoms: Diarrhea, abdominal pain, blood in stool, fatigue.
Treatment: Endoscopic procedures, medications, biologics.
Irritable Bowel Syndrome (IBS)
Symptoms: Alternating constipation and diarrhea, bloating.
Why see a GI specialist? To confirm diagnosis and manage symptoms effectively.
Celiac Disease
An autoimmune condition where gluten damages the small intestine.
Diagnosis requires blood tests and endoscopy.
Liver Disease
Includes fatty liver, hepatitis, cirrhosis.
Often silent until advanced, requiring specialist testing.
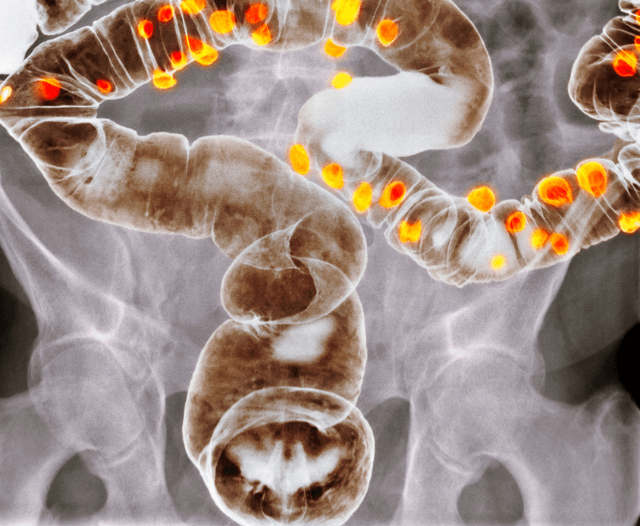
Colon Cancer & Polyps
Routine colonoscopies can remove precancerous polyps before they become cancerous.

What to Expect at Your Appointment
When you visit a gastroenterologist, you can expect:
- Detailed Medical History – including family history, lifestyle, and current symptoms.
- Physical Examination – abdominal check, blood pressure, weight.
- Diagnostic Tests – may include blood work, imaging (CT/MRI/ultrasound), stool tests, or endoscopic procedures.
- Treatment Plan – medication, dietary changes, minimally invasive procedures, or long-term monitoring.
Diagnostic and Treatment Procedures
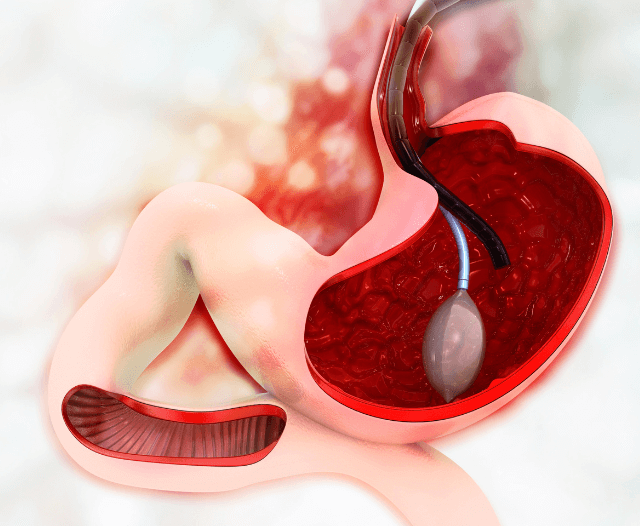
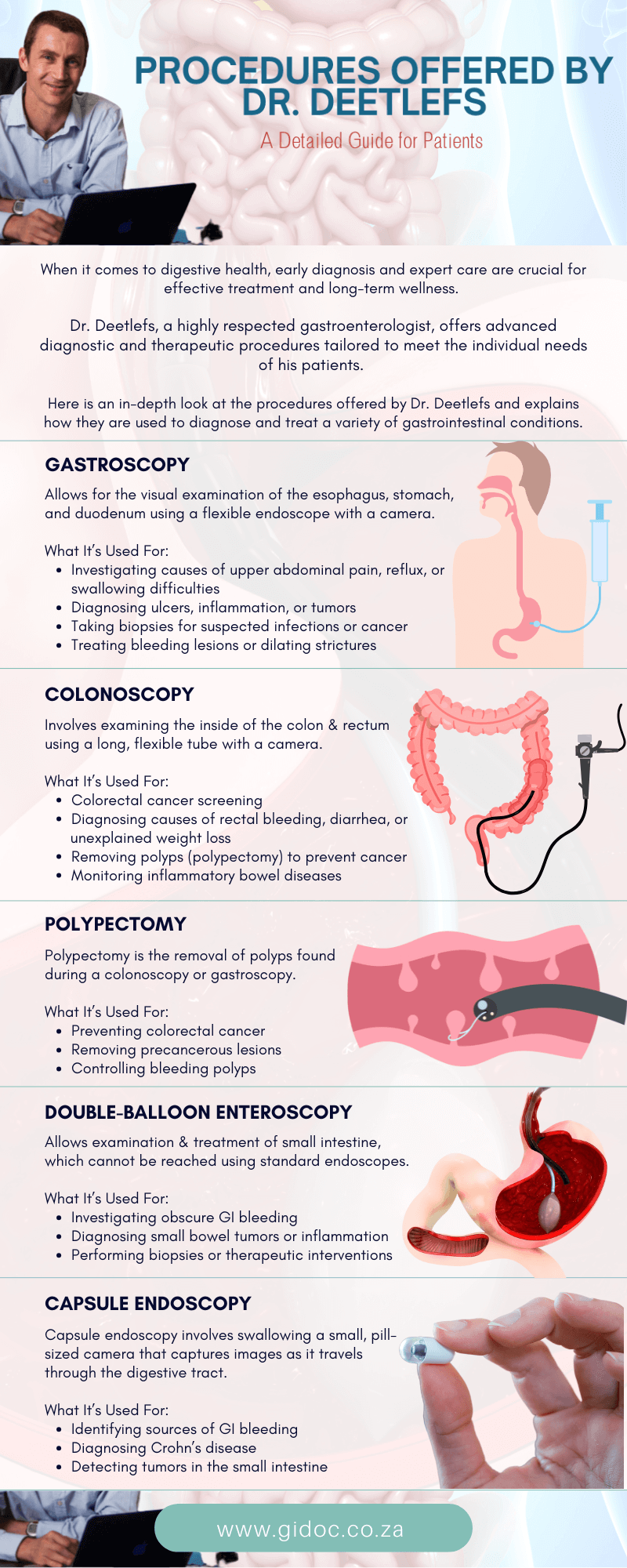
Gastroenterologists use advanced diagnostic tools:
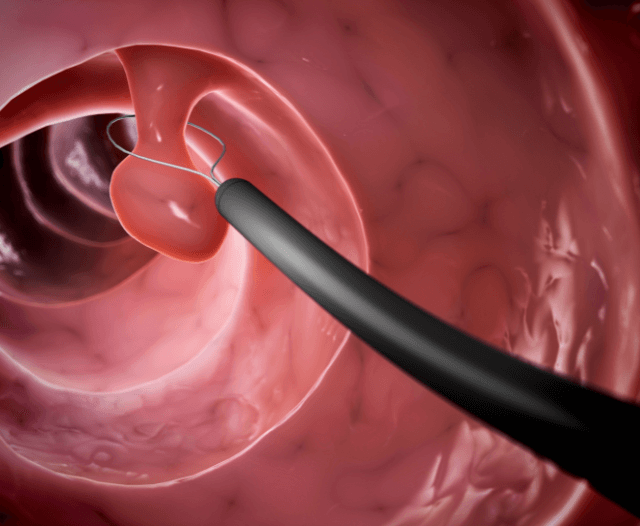
- Endoscopy: Examines the esophagus, stomach, and small intestine.
- Colonoscopy: Inspects the large intestine for polyps or cancer.
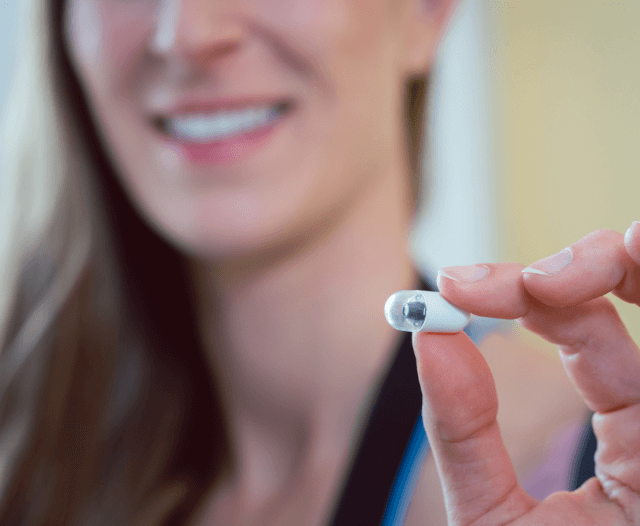
- Capsule Endoscopy: A small camera pill to view the small intestine.
- Endoscopic Ultrasound: Provides detailed imaging of digestive organs.
Endoscopic Dilatation or Stent Placement: Relieves strictures or obstructions.
Treatment approaches may include:
- Medications (acid reducers, anti-inflammatories, biologics).
- Lifestyle and dietary adjustments.
- Minimally invasive procedures for strictures, bleeding, or polyps.

The Importance of Early Detection
Ignoring symptoms can lead to serious complications:
- GERD may lead to Barrett’s esophagus and cancer.
- Untreated Crohn’s can cause strictures or fistulas.
- Delayed colonoscopy may allow cancer to progress undetected.
By consulting a gastroenterologist early, patients can prevent progression, receive appropriate treatment, and enjoy better quality of life.
When to Seek Emergency Care
Not all digestive issues can wait for an appointment. Seek emergency care if you experience:
- Severe abdominal pain with fever.
- Vomiting blood or passing black stools.
- Sudden, severe difficulty swallowing.
- Rapid, unexplained weight loss with weakness.
Conclusion
Your digestive system is central to your overall health, and ignoring warning signs can put you at risk of serious complications. From persistent heartburn and unexplained weight loss to routine screenings for cancer prevention, a gastroenterologist provides the expertise needed to diagnose, treat, and manage digestive conditions.
If you’re experiencing ongoing digestive symptoms—or if you’re due for a preventive screening—don’t wait.
Scheduling a visit with a gastroenterologist could be the most important step you take toward protecting your health.
Contact Dr. Deetlefs
Dr Eduan prides himself on his ability to help his patients to the best of his ability by embracing good listening skills, effective communication, compassion and knowledge and skill honed during years of private gastroenterology practice.
If you would like to book an appointment with a gastrointestinal (GI) specialist or would simply like more information on a particular GI topic, don’t hesitate to use our online booking form or call Dr. Deetlefs at 021 551 867.
DISCLAIMER: PLEASE READ CAREFULLY
The information on this website is to provide general guidance. In no way does any of the information provided reflect definitive medical advice and self-diagnoses should not be made based on information obtained online. It is important to consult a Gastroenterologist or medical doctor regarding ANY and ALL symptoms or signs including, but not limited to: abdominal pain, haemorrhoids or anal / rectal bleeding as it may a sign of a serious illness or condition. A thorough consultation and examination should ALWAYS be performed for an accurate diagnosis and treatment plan. Be sure to call a physician or call our office today and schedule a consultation.
© Dr. Eduan Deetlefs, Registered Gastroenterologist, GI Doc Cape Town
Our website information is not intended or implied to be a substitute for professional medical advice, diagnosis or treatment. Please consult a doctor about your specific condition. Only a trained physician can determine an accurate diagnosis and proper treatment.