The Importance of Routine GI Check-Ups
Introduction
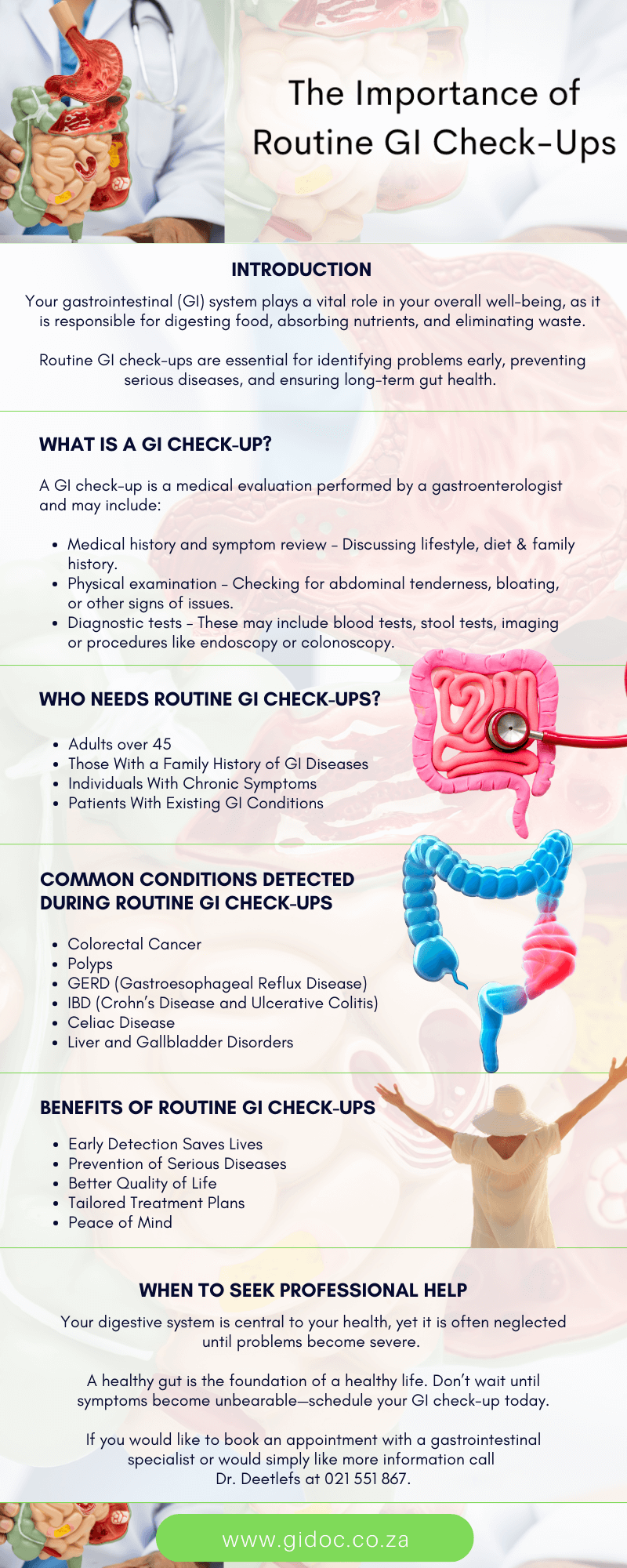
When it comes to health, most people think of regular visits to their general practitioner, dental check-ups, and even annual eye exams. However, one area often overlooked is digestive health. Your gastrointestinal (GI) system plays a vital role in your overall well-being, as it is responsible for digesting food, absorbing nutrients, and eliminating waste.
Routine GI check-ups are essential for identifying problems early, preventing serious diseases, and ensuring long-term gut health.
In this article, we’ll explore why these check-ups are so important, who should get them, what to expect, and how they can help prevent and manage common digestive conditions.
Why Digestive Health Matters
The gastrointestinal tract is a complex system that includes the esophagus, stomach, small intestine, large intestine (colon), rectum, liver, gallbladder, and pancreas. Each part plays a crucial role in breaking down food and delivering essential nutrients to the body.
When something goes wrong in this system, it doesn’t just cause digestive discomfort—it can affect your energy levels, immune system, and even mental health. For instance:
- Nutrient absorption issues can lead to vitamin deficiencies, fatigue, and weakened immunity.
- Chronic inflammation in the gut, such as with Crohn’s disease or ulcerative colitis, may increase the risk of colorectal cancer.
- Undiagnosed conditions, like celiac disease, can cause long-term damage if not identified and managed.
Routine GI check-ups are an important way to detect these issues early and keep the digestive system functioning properly.

What Is a GI Check-Up?
A GI check-up is a medical evaluation performed by a gastroenterologist—a doctor specializing in digestive health. Depending on your age, risk factors, and symptoms, a GI check-up may include:
- Medical history and symptom review – Discussing lifestyle, diet, and family history.
- Physical examination – Checking for abdominal tenderness, bloating, or other signs of issues.
- Diagnostic tests – These may include blood tests, stool tests, imaging (ultrasound, CT, MRI), or procedures like endoscopy or colonoscopy.
These evaluations can help diagnose conditions such as gastroesophageal reflux disease (GERD), ulcers, gallstones, inflammatory bowel disease (IBD), irritable bowel syndrome (IBS), and cancers of the digestive tract.
Who Needs Routine GI Check-Ups?
While anyone can benefit from digestive health screening, certain individuals are at higher risk and should be proactive about routine check-ups.
Adults Over 45
Colon cancer screening is now recommended for adults starting at age 45, as cases of colorectal cancer in younger adults are rising. Colonoscopy is the gold standard for detecting and removing polyps before they become cancerous.
Those With a Family History of GI Diseases
If you have a family history of colorectal cancer, Crohn’s disease, ulcerative colitis, or celiac disease, you may need earlier and more frequent check-ups.
Individuals With Chronic Symptoms
Persistent symptoms like abdominal pain, bloating, diarrhea, constipation, blood in the stool, or unexplained weight loss should not be ignored.
Patients With Existing GI Conditions
People with GERD, IBD, celiac disease, or liver conditions benefit from ongoing monitoring to prevent complications.

Common Conditions Detected During Routine GI Check-Ups
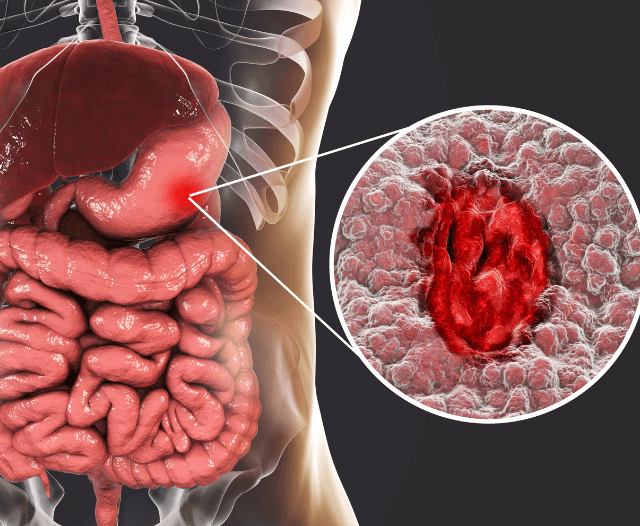
Colorectal Cancer
Colorectal cancer is one of the most preventable cancers when detected early. During a colonoscopy, gastroenterologists can remove polyps before they progress into cancer.
Polyps
These small growths in the colon can be benign but have the potential to turn cancerous if left untreated.
GERD (Gastroesophageal Reflux Disease)
Frequent acid reflux can damage the esophagus and increase the risk of Barrett’s esophagus, a precancerous condition.
IBD (Crohn’s Disease and Ulcerative Colitis)
Early diagnosis helps in managing inflammation, reducing flares, and preventing long-term complications like strictures and malnutrition.
Celiac Disease
Routine screening is important, especially if symptoms like bloating, diarrhea, or nutrient deficiencies are present.
Liver and Gallbladder Disorders
Fatty liver disease, gallstones, and hepatitis can often be picked up through routine blood work and imaging.
Benefits of Routine GI Check-Ups
Early Detection Saves Lives
The earlier a problem is caught, the easier it is to treat. For example, polyps removed during colonoscopy eliminate the risk of them turning into cancer.
Prevention of Serious Diseases
Many digestive conditions start small but worsen over time. Routine check-ups can stop disease progression before it becomes life-threatening.
Better Quality of Life
Managing digestive symptoms like bloating, constipation, or reflux improves comfort, sleep, and overall well-being.
Tailored Treatment Plans
Routine follow-ups allow gastroenterologists to adjust treatments based on changes in symptoms or test results.
Peace of Mind
Knowing your digestive health is being monitored provides reassurance and reduces anxiety.

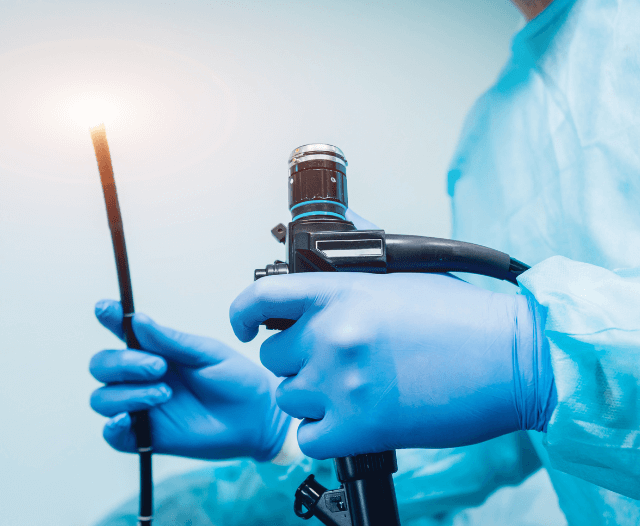
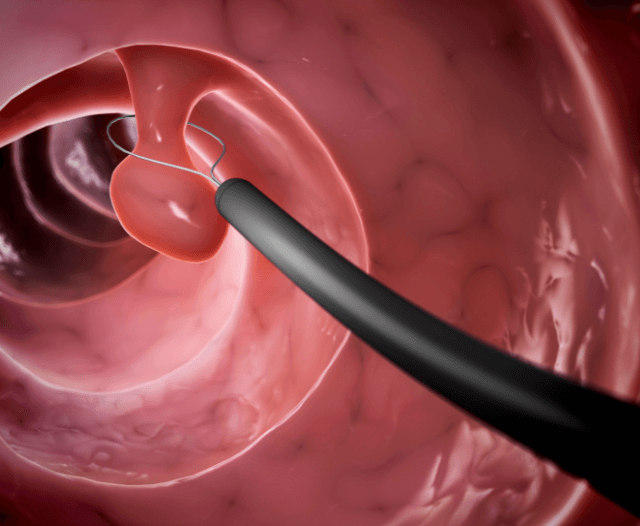
What to Expect During a Colonoscopy
One of the most common routine GI procedures is the colonoscopy. Here’s what happens:
- Preparation – Patients follow a special diet and take bowel-cleansing medications the day before.
- Sedation – You will be sedated to ensure comfort.
- Examination – The doctor inserts a flexible tube with a camera into the colon to look for polyps, inflammation, or other abnormalities.
- Polyp Removal – If found, polyps can be removed immediately.
- Recovery – Patients typically go home the same day.
Though often dreaded, a colonoscopy is quick, safe, and one of the most effective preventive tools in medicine.
Lifestyle and Routine Check-Ups: Working Together
While routine GI check-ups are essential, lifestyle changes can complement medical care and improve gut health:
- Eat a balanced diet rich in fiber, lean protein, and fermented foods.
- Limit processed foods, alcohol, and excess sugar that strain the digestive system.
- Stay hydrated to support bowel regularity.
- Exercise regularly, as physical activity helps digestion.
- Manage stress, which directly impacts the gut through the brain-gut connection.
Routine check-ups combined with healthy habits create a strong foundation for long-term digestive health.
Overcoming the Fear of GI Procedures
Many patients avoid routine GI check-ups due to fear, embarrassment, or misconceptions.
Common concerns include:
- Fear of discomfort – Sedation ensures that procedures like colonoscopy are painless.
- Embarrassment – Gastroenterologists perform these procedures daily and focus on patient health, not judgment.
- Concerns about cost – Preventive care is often more affordable than treating advanced disease.
Education and reassurance are key in encouraging patients to prioritize routine GI health screenings.

The Future of Routine GI Check-Ups
Advancements in gastroenterology are making routine check-ups even more effective and less invasive. Emerging technologies include:
- Capsule endoscopy – Swallowing a pill-sized camera that captures images of the digestive tract.
- Non-invasive stool DNA testing – Detecting colon cancer risk without a colonoscopy (though colonoscopy remains the gold standard).
These innovations promise greater accessibility, accuracy, and comfort for patients.
Conclusion
Your digestive system is central to your health, yet it is often neglected until problems become severe. Routine GI check-ups are one of the most powerful tools for preventing disease, improving quality of life, and ensuring early detection of potentially life-threatening conditions like colorectal cancer.
By staying proactive—especially if you are over 45, have a family history of GI disease, or suffer from persistent digestive symptoms—you can protect your gut health and overall well-being.
A healthy gut is the foundation of a healthy life. Don’t wait until symptoms become unbearable—schedule your GI check-up today.
Contact Dr. Deetlefs
Dr. Deetlefs has earned the reputation of a trusted health expert providing consultative, diagnostic, and therapeutic endoscopic and related services to patients in Cape Town and beyond.
Dr. Deetlefs can be contacted to confirm the estimated breakdown should you be interested in having the procedure done.
DISCLAIMER: PLEASE READ CAREFULLY
The information on this website is to provide general guidance. In no way does any of the information provided reflect definitive medical advice and self-diagnoses should not be made based on information obtained online. It is important to consult a Gastroenterologist or medical doctor regarding ANY and ALL symptoms or signs including, but not limited to: abdominal pain, haemorrhoids or anal / rectal bleeding as it may a sign of a serious illness or condition. A thorough consultation and examination should ALWAYS be performed for an accurate diagnosis and treatment plan. Be sure to call a physician or call our office today and schedule a consultation.
© Dr. Eduan Deetlefs, Registered Gastroenterologist, GI Doc Cape Town
Our website information is not intended or implied to be a substitute for professional medical advice, diagnosis or treatment. Please consult a doctor about your specific condition. Only a trained physician can determine an accurate diagnosis and proper treatment.