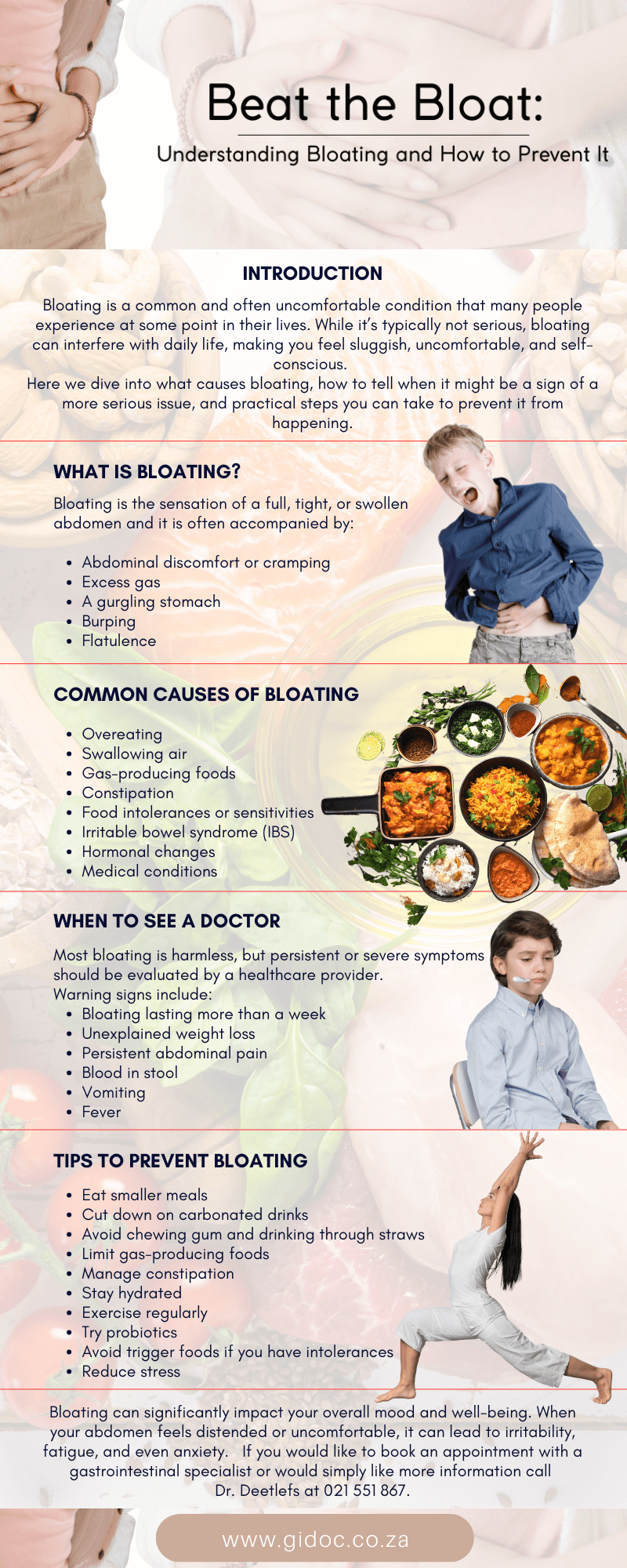
Beat the Bloat: Understanding Bloating and How to Prevent It
Bloating is a common and often uncomfortable condition that many people experience at some point in their lives. While it’s typically not serious, bloating can interfere with daily life, making you feel sluggish, uncomfortable, and self-conscious.
The good news? With the right understanding and lifestyle changes, bloating can often be prevented or managed effectively.
In this article, we’ll dive into what causes bloating, how to tell when it might be a sign of a more serious issue, and practical steps you can take to prevent it from happening.
What Is Bloating?
Bloating is the sensation of a full, tight, or swollen abdomen. Some people describe it as feeling like their stomach is stretched or filled with air. Bloating can be visible (with abdominal distension) or simply a feeling of internal pressure.
It is often accompanied by:
- Abdominal discomfort or cramping
- Excess gas
- A gurgling stomach
- Burping
- Flatulence
While occasional bloating is normal, frequent or severe bloating may point to an underlying gastrointestinal (GI) issue that needs medical attention.
Common Causes of Bloating
Understanding what’s behind your bloating is key to preventing it.
Here are some of the most common causes:
1. Overeating
Eating large meals too quickly can overwhelm your digestive system, causing excess gas production and bloating.
2. Swallowing Air
When you eat or drink too fast, chew gum, smoke, or drink carbonated beverages, you may swallow excess air, which gets trapped in the stomach and intestines.
3. Gas-Producing Foods
Some foods naturally produce more gas as they are broken down. Common culprits include:
- Beans and lentils
- Cruciferous vegetables (broccoli, cabbage, cauliflower)
- Onions and garlic
- Dairy (for those with lactose intolerance)
- Artificial sweeteners like sorbitol and xylitol
4. Constipation
When stool builds up in the colon, it can cause a backup of gas and lead to bloating.
5. Food Intolerances or Sensitivities
Lactose intolerance, gluten sensitivity, and other intolerances can cause bloating, diarrhea, and discomfort.
6. Irritable Bowel Syndrome (IBS)
IBS is a common GI disorder that often presents with bloating, gas, constipation, and/or diarrhea.
7. Hormonal Changes
Many women experience bloating before or during menstruation due to hormonal fluctuations affecting water retention and digestion.
8. Medical Conditions
Chronic bloating can be a symptom of conditions like:
- Celiac disease
- Small intestinal bacterial overgrowth (SIBO)
- Gastroparesis
- Inflammatory bowel disease (IBD)
- Ovarian cancer (rare, but persistent bloating should always be evaluated)

When to See a Doctor
Most bloating is harmless, but persistent or severe symptoms should be evaluated by a healthcare provider. Warning signs include:
- Bloating lasting more than a week
- Unexplained weight loss
- Persistent abdominal pain
- Blood in stool
- Vomiting
- Fever
These may point to a more serious condition that requires medical treatment or diagnostic testing.
10 Tips to Prevent Bloating
The good news is that for most people, bloating can be managed with simple lifestyle and dietary adjustments. Here are 10 effective ways to beat the bloat:
1. Eat Smaller, Slower Meals
Take time to chew your food thoroughly and avoid overeating. Eating slowly helps reduce the amount of air you swallow and gives your digestive system time to work effectively.
2. Cut Down on Carbonated Drinks
Sodas and fizzy drinks contain carbon dioxide, which contributes to gas buildup in your stomach. Opt for still water or herbal teas instead.
3. Avoid Chewing Gum and Drinking Through Straws
Both of these habits can cause you to swallow extra air, leading to bloating.
4. Limit Gas-Producing Foods
Keep a food diary to identify which foods cause bloating. Limit or avoid high-FODMAP foods (a group of fermentable carbs) if they trigger symptoms.
5. Manage Constipation
Keep your bowels moving with fiber-rich foods, regular exercise, and adequate water intake. If needed, talk to your doctor about fiber supplements or mild laxatives.
6. Stay Hydrated
Drinking enough water helps prevent constipation and promotes smoother digestion.
7. Exercise Regularly
Physical activity helps stimulate digestion and reduce bloating. Even a short walk after meals can make a difference.
8. Try Probiotics
Probiotics are beneficial bacteria that support gut health. They can help regulate digestion and may reduce bloating for some individuals. Yogurt, kefir, sauerkraut, and supplements are good sources.
9. Avoid Trigger Foods If You Have Intolerances
If you’re lactose or gluten intolerant, avoiding dairy or gluten-containing foods can significantly reduce bloating.
10. Reduce Stress
Stress affects your digestion through the brain-gut connection. Incorporate stress-reducing activities like yoga, meditation, deep breathing, or regular exercise into your routine.

Bloating Remedies That Can Help
If bloating does occur, there are several remedies you can try:
- Peppermint tea or capsules – Known to relax intestinal muscles and reduce gas
- Ginger tea or supplements – A natural anti-inflammatory that promotes digestion
- Simethicone tablets – Over-the-counter anti-gas medication
- Activated charcoal – May help absorb excess gas (talk to your doctor first)
- Heating pad – Applying heat to the abdomen can ease cramps and bloating
Special Considerations:
Bloating and Gut Health
Bloating can sometimes be a signal that your gut microbiome is out of balance. A healthy gut supports digestion, immunity, and overall well-being. Supporting your microbiome with prebiotics (fiber that feeds good bacteria) and probiotics can help reduce bloating and improve digestive health over time.
Examples of prebiotic-rich foods include:
- Bananas
- Oats
- Onions
- Asparagus
- Garlic
Combining these with fermented foods (yogurt, kimchi, kefir, miso) helps keep your gut bacteria thriving and your digestion efficient.

Final Thoughts
Bloating can significantly impact your overall mood and well-being. When your abdomen feels distended or uncomfortable, it can lead to irritability, fatigue, and even anxiety.
The physical discomfort may make it harder to focus, affect your appetite, and interfere with daily activities or social interactions.
In some cases, persistent bloating can contribute to body image concerns or lowered self-esteem, making it not just a physical issue but an emotional one as well. Addressing the root causes of bloating can help improve both your digestive health and your mental outlook.
Bloating is a common yet manageable condition that can be caused by everything from what you eat to how you eat. While it’s usually harmless, frequent or persistent bloating may signal an underlying issue that needs medical evaluation.
By taking simple steps like eating more mindfully, staying active, avoiding trigger foods, and supporting your gut health, you can enjoy a flatter, more comfortable belly — and better digestive health overall.
If your bloating doesn’t improve with lifestyle changes, consult with a gastroenterologist to rule out any serious conditions and get personalized advice.
Need Expert Digestive Care?
If you’re struggling with bloating, discomfort, or other digestive symptoms, consult a GI specialist for an accurate diagnosis and tailored treatment plan. Early evaluation can help prevent complications and improve your quality of life.
Dr. Deetlefs has earned the reputation of a trusted health expert providing consultative, diagnostic, and therapeutic endoscopic and related services to patients in Cape Town and beyond.
Dr. Deetlefs can be contacted to confirm the estimated breakdown should you be interested in having the procedure done.
DISCLAIMER: PLEASE READ CAREFULLY
The information on this website is to provide general guidance. In no way does any of the information provided reflect definitive medical advice and self-diagnoses should not be made based on information obtained online. It is important to consult a Gastroenterologist or medical doctor regarding ANY and ALL symptoms or signs including, but not limited to: abdominal pain, haemorrhoids or anal / rectal bleeding as it may a sign of a serious illness or condition. A thorough consultation and examination should ALWAYS be performed for an accurate diagnosis and treatment plan. Be sure to call a physician or call our office today and schedule a consultation.
© Dr. Eduan Deetlefs, Registered Gastroenterologist, GI Doc Cape Town
Our website information is not intended or implied to be a substitute for professional medical advice, diagnosis or treatment. Please consult a doctor about your specific condition. Only a trained physician can determine an accurate diagnosis and proper treatment.