What Is Dilatation of Strictures? A Patient’s Guide to Treatment and Recovery
When it comes to gastrointestinal health, early detection and treatment of narrowing in the digestive tract—also known as strictures—can significantly improve a patient’s quality of life.
Strictures can lead to uncomfortable and even dangerous symptoms such as difficulty swallowing, abdominal pain, or bowel obstruction. One of the most effective treatment methods for these conditions is dilatation—a minimally invasive procedure designed to widen narrowed areas of the gastrointestinal (GI) tract.
This guide will walk you through everything you need to know about the dilatation of strictures, from the causes and symptoms to the treatment process and recovery expectations.
Whether you’re a patient preparing for the procedure or simply seeking to better understand your treatment options, this article will provide a clear and compassionate overview of this important GI therapy.
What Are Strictures?
Strictures refer to abnormal narrowing in the gastrointestinal tract. This narrowing can occur anywhere along the digestive system, including the esophagus, stomach, small intestine, or colon.
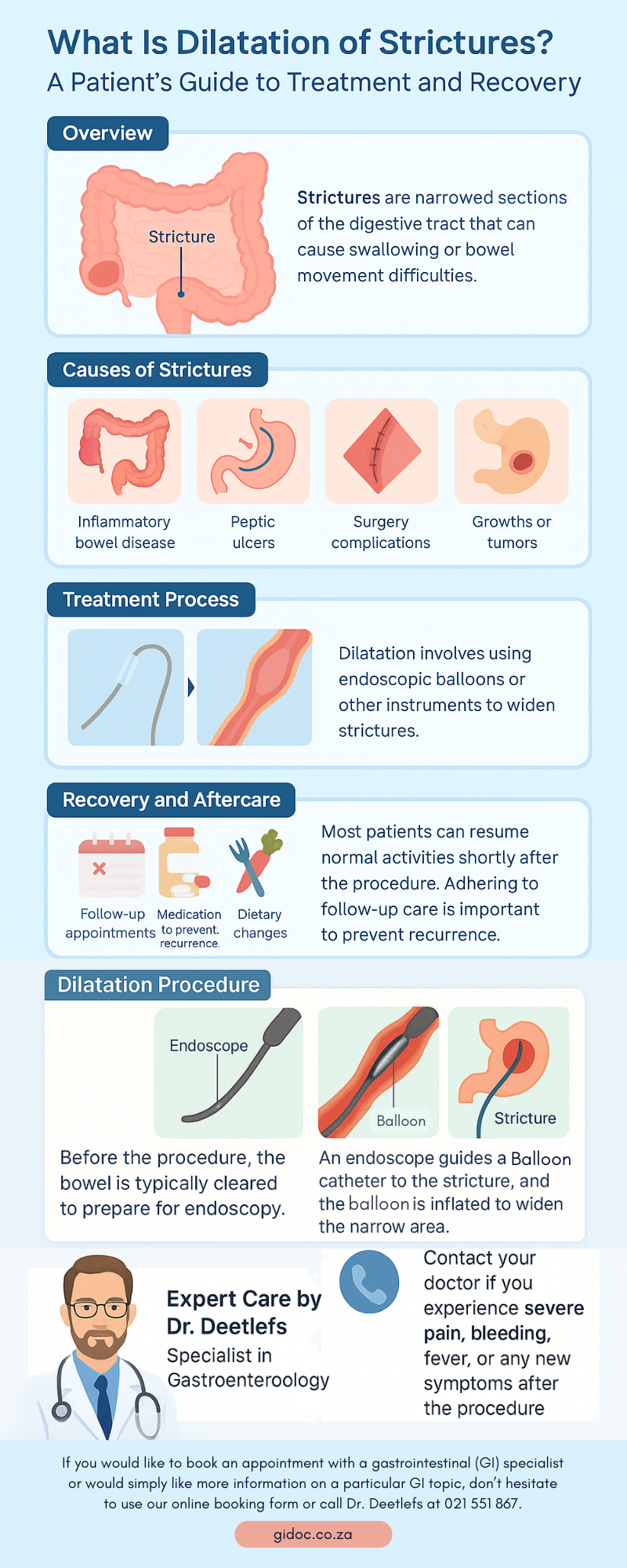
Strictures can be caused by various conditions, including:
- Gastroesophageal reflux disease (GERD)
- Inflammatory bowel diseases (IBD) like Crohn’s disease or ulcerative colitis
- Radiation therapy
- Surgical scarring
- Peptic ulcers
- Infections
- Cancer or tumors
- Prolonged use of nasogastric tubes or caustic injury
When the GI tract narrows, it restricts the movement of food, liquids, and digestive materials, often leading to symptoms that vary based on the stricture’s location.
Common Symptoms of GI Strictures
The symptoms of strictures largely depend on where they occur in the digestive system. Common signs include:
- Esophageal Strictures: Difficulty swallowing (dysphagia), food getting stuck, chest pain, and regurgitation.
- Gastric Strictures: Nausea, vomiting, bloating, early satiety, and weight loss.
- Small Bowel Strictures: Abdominal pain, cramping, nausea, vomiting, and signs of obstruction.
- Colonic Strictures: Changes in bowel habits, bloating, and abdominal discomfort.
If left untreated, strictures can lead to serious complications such as malnutrition, intestinal blockage, or perforation.
What Is Dilatation of Strictures?
Dilatation of strictures is a therapeutic procedure used to stretch or widen a narrowed segment of the GI tract.
This allows for the smoother passage of food and digestive contents, alleviating symptoms and improving the patient’s quality of life.
There are two main types of dilatations:
- Endoscopic Balloon Dilatation: A deflated balloon is inserted into the stricture site via an endoscope and then gently inflated to widen the narrowed area.
- Bougie Dilatation: A series of flexible, tapered tubes (called bougies) are inserted through the stricture, progressively increasing in size to expand the passage.
Both methods are typically performed under sedation or anesthesia and may be done as an outpatient procedure, depending on the patient’s condition.

Preparing for the Procedure
Before undergoing a dilatation, your gastroenterologist will perform a detailed assessment, which may include:
- Endoscopy: To visually inspect the stricture.
- Imaging Tests: Such as barium swallow, CT scan, or MRI to evaluate the severity and location.
- Biopsy: If cancer or inflammation is suspected.
Preparation instructions typically include:
- Fasting: No food or drink for at least 6–8 hours before the procedure.
- Medication Adjustments: Stopping certain medications like blood thinners or antiplatelet drugs.
- Medical History Review: Including allergies, previous surgeries, or anesthesia reactions.
What to Expect During the Procedure
1. Arrival and Sedation
Upon arrival, a nurse will check your vital signs, review your medical history, and start an IV line for medications. You’ll receive sedation to help you relax and minimize discomfort.
Your doctor will insert an endoscope (a thin, flexible tube with a camera) through your mouth or anus, depending on the location of the stricture.
3. Dilatation
Once the narrowed segment is located, the physician will use either a balloon or bougie to gently expand the area. The dilatation may last a few seconds to a couple of minutes.
4. Monitoring
After the procedure, you’ll be monitored in a recovery area until the sedation wears off. Most patients go home the same day.
Risks and Complications
Dilatation of strictures is generally safe, but like any medical procedure, it carries some risks. Potential complications include:
- Bleeding: Especially if the area is inflamed or ulcerated.
- Perforation (Tear in the GI wall): Though rare, this is the most serious risk and may require surgery.
- Infection
- Recurrence of the stricture
- To reduce these risks, it’s crucial to follow all pre- and post-procedure instructions and inform your healthcare provider of any underlying conditions or medications.

Post-Procedure Care and Recovery
Recovery after dilatation is typically smooth, especially if the procedure was performed without complications.
What to Expect Afterward
- Mild sore throat (if upper GI)
- Bloating or gas
- Slight cramping
- Temporary dietary restrictions
Most patients can resume normal activities within 24 hours, although you may need to stick to soft foods for a short period.
Follow-Up Care
- Repeat Procedures: Some patients may require more than one session to fully resolve the stricture.
- Ongoing Monitoring: Your doctor may recommend follow-up endoscopies, especially if the underlying condition is chronic (like Crohn’s disease).
- Medications: Anti-inflammatory drugs or acid reducers may be prescribed to prevent recurrence.

Managing the Underlying Cause
Successful treatment of strictures also means managing the root cause. Depending on your condition, your doctor may recommend:
- For GERD-related strictures: Proton pump inhibitors (PPIs) or surgical interventions.
- For IBD patients: Immunosuppressants or biologic therapies.
- For post-surgical strictures: Regular monitoring and additional dilatations if needed.
- For malignant strictures: Additional interventions like stent placement or surgery.
When to Call Your Doctor
After a dilatation, seek medical attention if you experience:
- Severe chest or abdominal pain
- Vomiting blood or passing black stools
- Fever or chills
- Difficulty swallowing or breathing
These could be signs of complications and should be addressed promptly.
Frequently Asked Questions (FAQs)
Q: Will I need multiple procedures?
A: It depends on the cause and severity of your stricture. Some patients achieve relief after one session, while others may need multiple treatments.
Q: Is dilatation painful?
A: The procedure is usually well-tolerated under sedation. Mild discomfort or a sore throat may occur afterward.
Q: How long does the effect last?
A: Duration varies. In some cases, the stricture can recur, especially if the underlying disease isn’t well-managed.

More About Dr. Deetlefs
Dr. Deetlefs is a highly respected specialist in the field of gastroenterology, known for his compassionate patient care and extensive expertise in a wide range of diagnostic and therapeutic procedures.
With years of clinical experience, he provides expert medical assistance in managing complex gastrointestinal conditions, including endoscopic treatments such as dilatation of strictures, colonoscopy, gastroscopy, and the placement of esophageal, gastric, and duodenal stents.
Dr. Deetlefs is dedicated to ensuring that each patient receives personalized care tailored to their unique needs, backed by the latest advancements in gastrointestinal medicine. His thorough approach, combined with a commitment to patient education, makes him a trusted figure in the journey toward better digestive health.
If you would like to book an appointment with a gastrointestinal (GI) specialist or would simply like more information on a particular GI topic, don’t hesitate to use our online booking form or call Dr. Deetlefs at 021 551 867.
Conclusion
Dilatation of strictures is a safe and effective procedure that provides significant relief from the symptoms caused by narrowed segments in the GI tract. Whether due to GERD, IBD, or post-surgical scarring, strictures can severely impact quality of life if left untreated.
With modern endoscopic techniques and tailored medical care, patients can expect improved function, reduced discomfort, and a path toward long-term digestive health.
If you are experiencing symptoms of a stricture or have been advised to undergo dilatation, speak with your gastroenterologist to fully understand your options. Early treatment and consistent follow-up are the keys to a smoother recovery and better health outcomes.
DISCLAIMER: PLEASE READ CAREFULLY
The information on this website is to provide general guidance. In no way does any of the information provided reflect definitive medical advice and self-diagnoses should not be made based on information obtained online. It is important to consult a Gastroenterologist or medical doctor regarding ANY and ALL symptoms or signs including, but not limited to: abdominal pain, haemorrhoids or anal / rectal bleeding as it may a sign of a serious illness or condition. A thorough consultation and examination should ALWAYS be performed for an accurate diagnosis and treatment plan. Be sure to call a physician or call our office today and schedule a consultation.
© Dr. Eduan Deetlefs, Registered Gastroenterologist, GI Doc Cape Town
Our website information is not intended or implied to be a substitute for professional medical advice, diagnosis or treatment. Please consult a doctor about your specific condition. Only a trained physician can determine an accurate diagnosis and proper treatment.